Researchers from Inserm, CNRS and the Université Joseph Fourier in Grenoble, in collaboration with Cambridge university, Strasbourg university and clinical practitioners from the Strasbourg University Hospital Centre, have analysed data from 17 comatose patients using functional MRI data. Their research reveals that the brain networks of these patients have been restructured. The results, published in PNAS on 26 November 2012, could help clinical practitioners diagnose comatose patients.
The researchers are focusing on analysing brain networks of brain-damaged comatose (non-traumatised) patients, a state where the individual is considered to be unconscious.
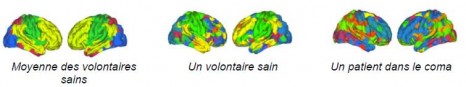
The authors of the study used an original graph theory-based methodology, where images were constructed using functional MRI data at rest and using robust statistical signal-processing methods. Local and overall effectiveness indices of functional brain networks were obtained for 17 brain-damaged patients and 20 healthy volunteers. Correlations in 417 brain regions were extracted to produce brain connection graphs using the statistically significant correlations.
Inserm unit 836 “Grenoble Institut des neurosciences”, CNRS researchers from the “GIPSA lab” and from the Behavioural and Clinical Neuroscience Institute in Cambridge, in collaboration with clinical practitioners from the Strasbourg University Hospital Centre, have been able to highlight restructured brain networks in brain-damaged (non-traumatized) comatose patients.
Through comparisons with the healthy subjects, the results demonstrate that the overall cerebral connectivity is preserved in comatose patients. By analysing the connectivity at a local level, the authors of the study have observed that some brain regions (“hubs”), which are highly connected in healthy volunteers, are less well connected in comatose patients. Conversely, the less densely connected regions in the network in healthy subjects become “hubs” in comatose patients.
Brain imaging obtained from connectivity graphs
Photos: © Sophie Achard – Petra Vertes
The connectivity graph method is used to summarize in a single image data acquired through MRI scanning. It translates the effectiveness of connections in a single region compared to all the others. By grouping the most interconnected regions, modules are revealed (each represented by a different colour). Patients and healthy volunteers both have different models in their spatial location, representing radical alterations to the brain connections.
According to current hypotheses, consciousness disorders in persistently comatose patients could be linked to disconnection phenomena between specific cortical regions, particularly the precuneus. The results of this study also point in this direction. “From an overall perspective, the topology of brain connections resists well to traumatism by reorganising the most interconnected regions in the network. It therefore seems that comas may be linked to changes in the location of “hubs” among the brain networks” suggests Chantal Delon Martin, an Inserm researcher.
An assessment of brain injury and comas
Patients with brain injury may go through various clinically-defined states: vegetative state that is characterized by the preserved sleep-wake cycle (eyes opening spontaneously, autonomous breathing, etc.); minimally conscious state where patients have partially preserved environmental consciousness (eye movement capacity, reaction to stimulation); locked in syndrome where the patient is paralysed but conscious (communication using eyes); brain death when the coma is irreversible flat line EEG, no blood flow).
Coma (from the Greek κῶμα kôma meaning “deep sleep”) is one of the different states where self awareness and consciousness of the outside world is eradicated further to an accident (cerebral, cardiac, etc.). There are two coma phases: the “acute” coma phase (a few days after the accident) and the “chronic” phase (one month or more). Brain restructuring was observed by researchers during the “acute” phase, when it is not known which coma type the patient will develop.
Assessments of brain injuries in comatose patients are currently conducted through clinical examination, morphological MRI, evoked potentials and by SPECT (Single-photon emission computed tomography) or TEP (Positron emission tomography (PET). “The results of this study could help clinical practitioners in the difficult diagnosis process for comatose patients, since this method makes it possible to characterize each patient individually”, conclude the researchers.