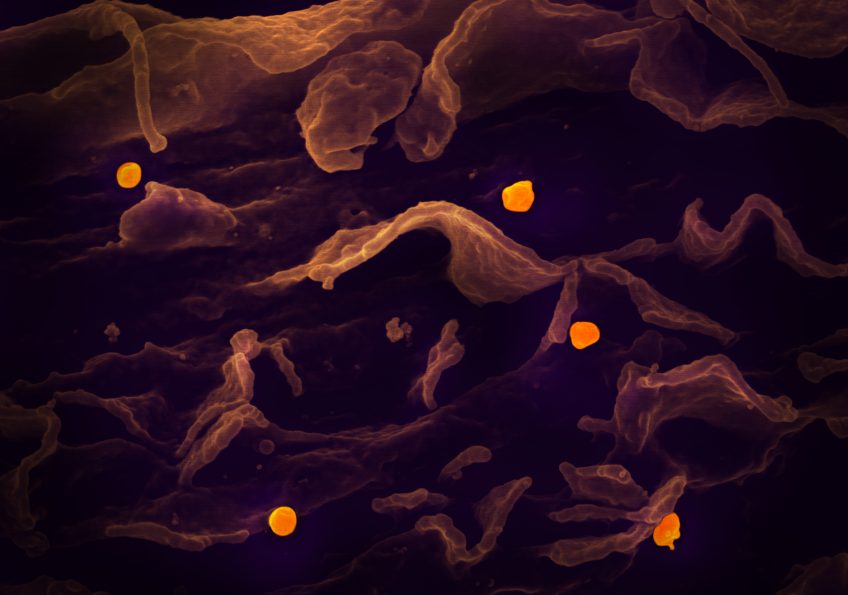
 A scanning electron micrograph shows the Nipah virus (yellow) budding from the surface of a cell.© National Institute of Allergy and Infectious Diseases, NIH
A scanning electron micrograph shows the Nipah virus (yellow) budding from the surface of a cell.© National Institute of Allergy and Infectious Diseases, NIH
The WHO recently classified the Nipah virus (NiV) as one of the eight main emerging pathogens likely to cause major epidemics in the future. In a context where no treatment or vaccine is yet available, a team comprising researchers from Inserm (Unit 955-VRI) and from the Université Paris-Est Créteil (UPEC) is presenting the preclinical results of an innovative vaccine against this virus. Most candidate vaccines target the viral surface proteins required for entry into human cells. To develop its new vaccine, the team at the VRI (Vaccine Research Institute of the ANRS MIE/Inserm) focused on the central role played by antigen-presenting cells (APCs) in the development of protective responses. The candidate vaccine, called CD40.NiV, carries specific parts of the surface proteins of the NiV-B virus, the Bangladesh strain. Following infection with the Nipah virus in animals, CD40.NiV demonstrated immunogenicity, neutralisation and complete protection, representing an important step towards the clinical development of a vaccine against the infection. The results of this work have just been published in the March 2024 issue of Cell Reports Medicine.
The Nipah virus (NiV) is a zoonotic virus, meaning it is transmitted from animals to humans. However, it can also be transmitted via contaminated food or directly between individuals. The clinical presentation can range from asymptomatic infection to acute respiratory infection to fatal encephalitis. First identified in Malaysia in 1999, the virus has since spread regularly through outbreaks in Bangladesh and India. Mortality linked to these outbreaks is estimated to be between 75% and 90%.
The virus has recently been included on the WHO list of priority emerging pathogens. There is currently no approved treatment or vaccine. Numerous candidate vaccines are under study or development. Most target the G and F proteins on the surface of the virus, which are necessary for it to enter human cells and spread throughout the body.
The teams at Inserm and UPEC have developed an original approach involving antigen-presenting cells (APCs), in particular dendritic cells, which play an important role in the immune response. To construct the CD40.NiV vaccine, specific parts (or epitopes) of the G, F and N proteins of the Bangladesh strain of Nipah virus (NiV-B) were attached to an antibody recognising the CD40 receptors on the surface of dendritic cells. The epitopes are thus presented directly to the cells of the immune system.
Immunogenicity (the ability to induce an immune response) of the vaccine was assessed in mice and non-human primates after two administrations of CD40.NiV vaccine (the so-called “prime-boost” strategy). As early as 10 days after the first vaccination with CD40.NiV (prime), NiV-specific IgG and IgA antibodies, as well as neutralising antibodies (specific antibodies that prevent infection by blocking viral entry into target cells) were produced. The neutralising antibody response is maintained for at least 100 days after the peak of the immune response. In addition, the team showed that the antibodies induced against NiV also neutralise various strains of NiV (Malaysia, Cambodia) and the Hendra virus (this is known as cross-neutralising immunity), an infectious agent transmitted by bats and causing a highly fatal infection in horses and humans.
To ensure that the vaccine was effective, the animals were infected with the NiV virus 60 days after the second injection of CD40.NiV (boost). Protection was complete.
This preclinical study demonstrated that the CD40.NiV vaccine candidate confers protection against the development of Nipah virus, with 100% survival of immunised animals until the end of the study, 28 days after infection. The absence of significant clinical signs or virus replication suggests that the candidate vaccine provides ‘sterilising immunity’, meaning that it can prevent the disease and its transmission.
Overall, results obtained with CD40.NiV are highly promising for fighting NiV infection and represent an important milestone towards the clinical development of a vaccine against this virus.
These contents could be interesting :
A vaccine targeting antigen presenting cells through CD40 induces protective immunity against Nipah disease.
Cell Reports Medicine, 11 mars 2024
https://doi.org/10.1016/j.xcrm.2024.101467
Pastor Y (1, 2), Reynard O (3), Iampietro M (3), Surenaud M (1, 2), Picard F (1, 2), El Jahrani N (1, 2), Lefebvre C (1, 2), Hammoudi A (1, 2), Dupaty L (1, 2), Brisebard E (4), Reynard S (3, 5), Moureaux E (6), Moroso M (7), Durand S (3), Gonzalez C (3), Amurri L (3), Gallouet A-S (8), Marlin R (8), Baize S (3, 5), Chevillard E (7), Raoul H (7), Hocini H (1, 2), Centlivre M (1, 2), Thiébaut R (2, 9, 10), Horvat B (3), Godot V (1, 2), Levy Y (1, 2, 11)*, Cardinaud S (1, 2)*.
- Inserm U955 – Équipe 16, Vaccine Research Institute (VRI), Institut Mondor de Recherche Biomédicale (IMRB), Université Paris-Est Créteil (UPEC), Créteil, France
- Vaccine Research Institute (VRI), Créteil, France
- Centre International de Recherche en Infectiologie (CIRI), Université de Lyon, INSERM U1111, Ecole Normale Supérieure de Lyon, Université Lyon 1, CNRS UMR5308, Lyon, France
- INRAE Oniris UMR0703, APEX, Nantes, France
- Unité de Biologie des Infections Virales Émergentes, Institut Pasteur, Lyon, France
- BioPRIM, Baziège, France
- Laboratoire P4 INSERM–Jean Mérieux, INSERM US003, Lyon, France
- Center for Immunology of Viral, Auto-immune, Hematological and Bacterial diseases (IMVAHB/IDMIT), Université Paris-Saclay, Inserm, CEA, Fontenay- aux-Roses, France
- Bordeaux, Department of Public Health, Inserm Bordeaux Population Health Research Centre, Inria SISTM, Bordeaux, France
- CHU Bordeaux, Department of Medical information, Bordeaux, France
- Assistance Publique-Hôpitaux de Paris, Groupe Henri- Mondor Albert-Chenevier, Service Immunologie Clinique, Créteil, France
* Co-auteurs

