
© Inserm/F.Koulikoff
Chronic diseases are long-term and sometimes permanent noncommunicable conditions that change over time. According to the World Health Organization (WHO), they are the world’s leading cause of mortality and in Europe “contribute to around 86 % of deaths (…) and represent an increasing burden on healthcare systems, economic development and wellbeing of a large proportion of the population, particularly those aged 50 or above”.
In France, the proportion of those aged 60 or above is expected to increase from one quarter of the total population in 2015 to one third in 2040. Currently, one in four French people has a chronic disease, which increases to three in four beyond the age of 65. With the increase in life expectancy, the number of older adults with chronic diseases is on the up. These are conditions that lead to functional limitations with impacts on quality of life, with the number of dependent individuals expected to rise from 1.2 million in 2012 to 2.3 million in 2060. By improving the prevention and management of chronic diseases, we are therefore taking steps to tackle a major public health emergency.
According to the WHO report of 2010, a large percentage of chronic diseases is responsive to prevention if four primary risk factors are addressed: tobacco use, physical inactivity, alcohol consumption and unhealthy diet. In France, current estimations set the direct (75 %) and indirect (25 %) costs of physical inactivity in the region of €1.3 billion.
Prevention measures can be implemented prior to development of the diseases and at any time during their progression. Given that chronic diseases and their complications contribute very strongly to a state of dependency, preventing their complications and recurrence represents a key challenge for the maintenance of autonomy, notably in older adults.
Inserm was tasked by the French Ministry of Sports with producing a collective expert review in order to take stock of scientific knowledge and to analyze, within the scope of chronic diseases, the impact of physical activity[1] and its place in the care pathway. This review is based on a critical analysis of the international scientific literature made by a multidisciplinary group of thirteen researchers with expertise in various fields relating to chronic diseases, from sports medicine to psychosociology.
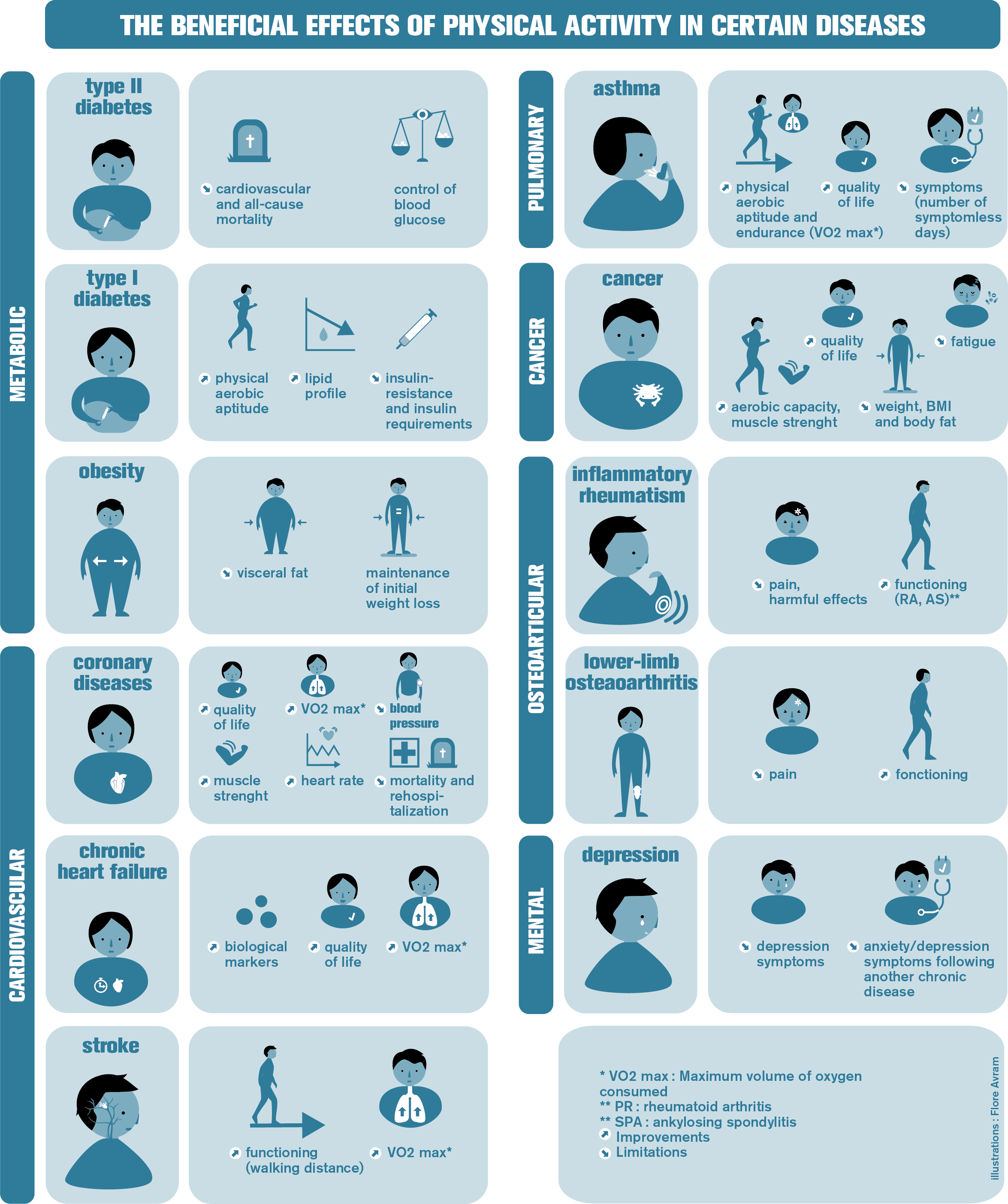
The main conditions studied were cardiovascular diseases, cancer, diabetes and chronic respiratory diseases. Obesity, a determinant of chronic diseases and morbid phenomenon in itself, was also included, as were certain mental disorders (depression, schizophrenia), musculoskeletal disorders and multimorbidity.
The research presented in this review comes with three major challenges.
The first is not so much about knowing whether we should recommend regular adapted physical activity for chronic disease sufferers – there is no longer any doubt on the need for this – but rather determining the most efficient program characteristics according to patient physical aptitudes and psychosocial resources, in order to obtain maximum benefit with minimum risk: when should the program begin, what kind of physical activity should it include, at what intensity, how often, in what environment and with what kind of intervention?
The second involves identifying what determines the adoption of behavior that is active, maintained over the long-term and compatible with patient lifestyles. After all, what would be the point of a physical activity program whose efficacy was demonstrated by a clinical trial conducted under ideal conditions, but which turns out to be unsuitable for and ignored by patients?
The third challenge is about understanding the mechanisms through which physical activity acts in general, by improving the physical condition, and also specifically according to the diseases concerned. A large part of the review describes for each disease the benefits/risks of physical activity, and its utility in terms of prevention, treatment and additional care.
The expert group uses these scientific elements as a basis on which to establish recommendations for research as well as recommendations for health authorities in terms of measures to take.
Principal recommendations
- Prescribe physical activity for all the chronic diseases studied and include it in the care pathway
While rest has long been the rule in many chronic diseases, we are now seeing a genuine paradigm change with scientific studies showing that, when physical activity recommendations and disease-related complications are taken into account, not only does exercise not worsen the condition but that it is also more beneficial the sooner after diagnosis it is introduced.
Consequently, the expert group considers that physical activity forms an integral part of the treatment of chronic diseases. It recommends its systematic prescription, as early as possible in the care pathways of the diseases studied. It also recommends its prescription prior to any drug treatment in mild to moderate depression, type 2 diabetes, obesity and lower limb peripheral arterial disease.
The expert group has also prepared the following recommendations which, although specific to each disease, do agree on the frequency of adapted physical activity – namely a minimum of three sessions per week.
Here are some examples:
- obesity: place the emphasis on waist size reduction as a follow-up parameter rather than weight loss and suggest endurance activity programs;
- type 2 diabetes: opt for muscle strengthening combined with endurance activities of moderate to strong intensity;
- coronary diseases: perform regular endurance activities which can be optimized by adjusting the intensity of the exercise;
- lower-limb peripheral arterial disease: the first-line treatment is walking;
- heart failure: irrespective of disease severity, all patients can benefit from an effort retraining program, thanks to regular and gradual training. Ideally, 30 minutes of moderate activity five times per week in the last phase of the program, which must be life-long;
- stroke: reduce the impact of neuromuscular sequelae on patient quality of life and prevent relapse by improving cardiorespiratory capacity and muscle strength through regular physical activity that incorporates the practice of daily techniques;
- chronic obstructive pulmonary disease (COPD): improve quality of life and reduce complication-related functional limitations through varied and long-term regular physical activity (endurance, muscle strengthening, swimming, tai chi…);
- asthma: reduce the intensity and frequency of attacks by improving VO2max, endurance and exercise capacity through endurance activities;
- osteoarticular diseases: prevent and/or reduce pain and incapacity through varied and adapted physical activity programs, maintained over the long-term;
- cancer: improve quality of life and reduce disease and treatment-related side effects (muscular deconditioning, fatigue, treatment intolerance…) and recurrence by offering programs combining endurance and muscle strengthening;
- depression: prevent recurrence and improve symptoms through programs combining endurance and muscle strengthening.
- Adapt the prescription to patient individual and medical characteristics
The principal barriers to physical activity are generally related to the disease itself (pain, fatigue, side effects of certain treatments…).
The main challenge therefore is to adapt the physical activity to the patient’s health, treatment, physical capacity, medical risks and psychosocial resources.
The expert group recommends:
- evaluating patient physical activity level through an interview and/or simple tests (e.g. the 6-minute walk test) to evaluate capacity and tolerance for exercise. More complex tests (e.g. cardiopulmonary exercise testing) are required to adapt the prescription in terms of intensity of activity and make it safe for the most vulnerable individuals;
- monitoring changes in physical condition and exercise tolerance in order to adapt the prescription;
- individualizing the prescription of physical activity by taking into account its context and type, its conditions (intensity, duration, frequency), and above all patient preferences and expectations that influence their interest and pleasure in performing this type of activity;
- proposing personalized programs to individually adjust physical activity according to the disease, the patient and their environment in order to promote adherence and compliance, particularly over the long-term.
- Structure the patient pathway to encourage physical activity at all stages of the disease
A physical activity project must take the entire patient pathway into account. From the very beginning of treatment, it is important to devise the preparation and identification of the elements enabling the patient to pursue physical activity in or close to their home. It is about enabling the patient to immediately mobilize their capacities and if they wish, to play an active role in their care pathway.
- Incorporate an educational approach to promote patient commitment to a physical activity project over the long-term
The main challenge is for the patient to make physical activity part of their daily life, which from the outset involves encouraging their commitment to and the development of their autonomy in an activity that is meaningful for the patient and which they can pursue over the long-term. The correct incorporation of physical activity in the overall treatment and therapeutic education project means regular communication between the adapted physical activity professional and the healthcare team.
The expert group recommends combining the programs of physical activity with programs of therapeutic education and initiating any intervention with a shared educational assessment which invites the patient to identify their life habits, needs, possibilities, desires, obstacles and incentives, and how they would like to be helped… Then an objective should be set and the resources that they will mobilize to achieve that objective identified. Follow-up assessments will make it possible to adjust the objectives and renew the resources throughout the program.
For patients presenting characteristics known to limit or compromise adherence and long-term maintenance of the activity (older age, low socioeconomic level, social precariousness…) and/or with little or no experience of physical activity, the expert group recommends a professionally-supervised educational cycle of adapted physical activity of several months’ duration. The challenge being to enable these patients to experience physical activities appropriate to their possibilities and needs, to feel and get pleasure from the effects and recognize them as being beneficial to their health.
Once the patient has the resources, the expert group then recommends supporting them in building a physical activity project which has meaning for their care pathway and life.
5. Support patient motivation in implementing their project
Suggesting forms of physical activity that are not just effective but also fun and motivating needs to remain an ongoing concern. The commitment of individuals with chronic diseases to regular physical activity is primarily motivated by the pleasure and utility they find in it and also by their beliefs in terms of perceived benefit for their physical health and psychological wellbeing. Inversely, a lack of knowledge of the positive effects of physical activity or negative beliefs according to which it would be useless in managing their condition, may underlie any failure to initiate or maintain this activity.
Patients can also be motivated by the positive self-image generated by physical activity (or the negative view they would have of themselves in its absence). More particularly, having to take oneself in hand in order to face the disease in question is seen by some as a responsibility or a duty.
While intentions and planning are generally an unavoidable stage in establishing physical activity, routines need to be created for it to be adopted over the long-term. To encourage the long-term maintenance of motivation, the expert group recommends using a combination of strategies, which include communicating information on the effects of physical activity and the opportunities for engaging in it, the definition of objectives, the follow-up and anticipation of barriers and obstacles to its pursuit, the social support and sharing of experiences, cognitive reassessment and motivational interviewing.
These strategies have a greater effect on motivation when several of them are used together. They can be used by various stakeholders throughout the care pathway (nursing staff, doctors, psychologists, adapted physical activity specialists…) during individual or group face-to-face sessions. Some strategies may benefit from technological support (accelerometer, social media, websites, telephone calls, text messages, connected health objects, serious games, videoconferences…).
- Train doctors in the prescription of physical activity
Training in the theoretical and practical knowledge of the benefits of physical activity and of the physical activity intervention initiatives is required for all healthcare professionals.
As a consequence, the expert group recommends:
- the widespread implementation of mandatory modules relating to the prescription of physical activity during the training of medical students;
- the continuing education of doctors with the same objectives as those of the initial training;
- the participation of experts in health-promoting physical activity as well as experts in adapted physical activity in these multidisciplinary training modules;
- the development of dialogue and joint deliberation among the various professions involved in favor of the practice of adapted physical activity.
- Train physical activity professionals in knowledge of the disease and in incorporating physical activity in the medical intervention
The expert group recommends training adapted physical activity specialists in how to:
- control the interactions between the physical activity and the chronic disease when devising programs and sessions for patients;
- implement and interpret specific physical activity tests (in addition to medical tests) in line with individual limitations;
- implement a shared educational assessment to engage the patient in a project approach and evaluate with them their motivation and obstacles in terms of physical activity, their life habits and conditions and possibilities for activity;
- devise and plan a physical activity program that develops individual autonomy and that is appropriate to the medical contraindications and indications, to the capacities and limitations of the individual, to their level of physical activity and their objectives;
- implement intervention programs by adjusting the physical activity to the progression of the individual and to the changes in their state of health on the basis of relevant evaluations;
- develop an education for health or therapeutic education approach according to the level of qualification and/or the stage of the care pathway at which the intervention takes place;
- mobilize techniques to support patient motivation and commitment to their personal project;
- communicate with the patient and the various players implicated in the personalized pathway in respect of the rules of confidentiality;
- manage, implement and incorporate the principles of patient-caregiver relationship ethics when working with the patient;
- manage the practice of physical activity in conditions of safety by individuals living with a chronic disease.
- Promote research
- Into the conditions of the intervention and their effects
Few studies evaluate the conditions of maintaining physical activity over the long-term, in a “real-world” environment. Yet a patient with a chronic disease has to face potential side effects or sequelae of the treatments and manage the progression of their disease as they get older. This can take the form of the development of other diseases (comorbidities), anxiety or depression symptoms or neurocognitive dysfunction. Getting patients with chronic diseases to adopt new behaviors requires the precise definition of what is at stake in the psychological adjustment to this type of disease.
The expert group recommends consolidating research concerning the feasibility, benefit-risk balance, adherence over the long term to physical activity and in particular it recommends studying the conditions necessary to maintain it, especially during the transition phases (from the hospital to the follow-up and rehabilitation care center, from the center to community medicine, from community medicine to home) and to study the intervention initiatives.
- Into the methods of incorporating physical activity in the care pathway and its purposes
It is about pinpointing the meaning that physical activity can have for the patient during their disease, analyzing the impact on its conduct by interactions with healthcare professionals, peers, family members, and by identifying the conditions enabling the patient to establish new parameters for living.
- Into motivation and compliance over the long-term
- Into the technological tools
The expert group recommends evaluating the technological tools and testing their efficacy in order to estimate the benefit of their incorporation in the patient pathways.
The innovations and prevention interventions which do not take social health inequalities into account often help make them worse[2]. Consequently, the expert group recommends conducting studies to analyze the cost-effectiveness of these new technologies according to patient culture, age, sociocultural level and expectations.
- Into the effects of the public health policies in favor of physical activity by individuals with chronic diseases
The French national “Sport, health and well-being” plan has produced new partnerships in the 22 regional territories, helping to develop a physical activity offering with the purpose of preventing chronic diseases. By developing the prescription by treating physicians of adapted physical activity for patients with chronic diseases, article 144 of the French public health law and the tools accompanying it, are targeting the widespread implementation of this type of prescription. This raises the question of the accessibility to this treatment or prevention provision for all sufferers of chronic diseases, irrespective of their age, geographical area of residence or their socioeconomic and cultural resources.
The expert group recommends studying the construction of the medical prescription of physical activity and its impact on social inequalities in health, examining also how covering its cost would affect patient take-up of the programs and their commitment over the long-term.
- Into the physiological action mechanisms of physical activity, in general and for each disease
- Into the synergic effects of strategies combining diet and physical activity
[1] Inserm Collective Expert Review. Social inequalities in health linked to diet and physical activity, 2014
[2] WHO defines physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure”.
Since its creation in 1993, Inserm’s Collective Expert Review has been entrusted with a mission of expert review and knowledge transfer for many institutional bodies and decision-makers (Ministries, Agencies, etc.) in the area of public health.
This mission, performed by the Collective Expert Review Unit attached to the Thematic Institute for Public Health, provides scientific insight to assist decision-making in matters of public policy on health. The Collective Expert Review Unit ensures the scientific framework, bibliographic support, coordination and promotion of collective expert reviews.
Having accumulated widely-renowned experience and know-how, Inserm’s Collective Expert Review currently occupies a unique position in the field of health-related expert review. The expert review procedure relies on the scientific competences of expert researchers and clinicians representing all disciplines useful to public health, gathered into ad hoc working groups by the Collective Expert Review Unit. In a constant drive for scientific excellence, independence and relevance in relation to scientific, economic and social issues raised by the themes addressed, the reviews contribute to the social application of the sciences. Experts are chosen within the French-speaking scientific community for their scientific competences (as evidenced by their publications) and for their independence.
Collective expert reviews, published in book form, address important issues such as health and environment, occupational health, aging, nutrition, addictive behaviors, disabilities, etc. Many of these reports provide a summary and recommendations, available online as soon as the results of the expert review are published. The complete book is available in bookshops and online in the months following publication.
The expert review “Physical activity. Prevention and treatment of chronic diseases”, has taken over 3 years of work and the critical analysis of approximately 1,800 scientific documents.
[/complement]
These contents could be interesting :
Groupe d’experts ayant réalisé cette expertise collective :
Julie BOICHE, Laboratoire Epsylon EA 4556, Université Montpellier 1
François CARRE, Laboratoire Traitement du signal et de l’image (LTSI) UMR Inserm 1099, Université de Rennes 1
Béatrice FERVERS, Département Cancer et Environnement, Centre Léon Bérard
Damien FREYSSENET, Laboratoire de Physiologie de l’Exercice – EA4338, Faculté de Médecine, Campus santé Innovation
Isabelle GREMY, ORS Ile-de-France
Thibaut GUIRAUD, Institut des maladies métaboliques, CV I2MC, Inserm UMR1048 Toulouse, Clinique Cardiocéan
Cédric MORO, Inserm UMR1048 Institut des maladies métaboliques, CV (I2MC), CHU Rangueil
Christelle NGUYEN, et Serge POIRAUDEAU†, Hôpital Cochin, Service de Rééducation et de Réadaptation de l’Appareil Locomoteur et des Pathologies du Rachis, INSERM UMR-S 1124 – Toxicologie, Pharmacologie et Signalisation Cellulaire, Université Sorbonne Paris Cité
Grégory NINOT, Université de Montpellier, Epsylon EA4556, Plateforme Universitaire CEPS
Claire PERRIN, UFR Staps, CRIS-EA647/AP et Vulnérabilité, Université Claude Bernard Lyon 1
Alain VARRAY, Laboratoire Movement to Health (M2H), Neuroplasticité et réhabilitation, Université de Montpellier, EuroMov
Agnès VINET, Laboratoire de Pharm-Ecologie Cardiovasculaire (LAPEC) EA 4278, Université d’Avignon, Pôle sportif universitaire et de recherche
Guillaume WALTHER, Laboratoire de Pharm-Ecologie Cardiovasculaire (LAPEC) EA 4278, Université d’Avignon, Pôle sportif universitaire et de recherche
La coordination de cette expertise a été assurée par le Pôle d’expertise collective de l’Inserm rattaché à l’Institut thématique de Santé publique.
Cette expertise est publiée sous le titre «Activité physique. Prévention et traitement des maladies chroniques »
Éditions EDP Sciences, janvier 2019, 824 pages, 70 euros
Collection Expertise collective
Lien vers la synthèse accessible en ligne sur www.inserm.fr

