Researcher Contact
Léon Kautz
Inserm staff scientist
Unit 1220 Inserm/INRAE/ENVT/Université Toulouse III – Paul-Sabatier, Digestive Health Research Institute
Email: yrba.xnhgm@vafrez.se
Telephone number available on request
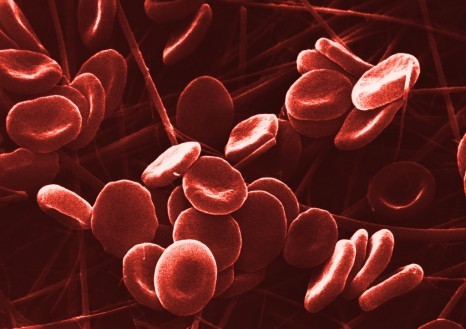 An essential component of the haemoglobin in red blood cells, iron is crucial to many biological processes – including the transport and storage of oxygen in the body. © Inserm/Claude Féo
An essential component of the haemoglobin in red blood cells, iron is crucial to many biological processes – including the transport and storage of oxygen in the body. © Inserm/Claude Féo
Anaemia is a major public health problem worldwide, affecting around one third of the population. Its causes are multiple, but the most common are a lack of red blood cell production, a lack of iron in the blood, and genetic diseases such as thalassaemia. A better understanding of iron metabolism is essential to improve the care of the many patients affected. In a new study, Inserm researchers at the Digestive Health Research Institute (Inserm/INRAE/Université Toulouse III – Paul-Sabatier/Toulouse National Veterinary School) identified the major role of a protein called FGL1 in iron metabolism. Their discovery paves the way for new clinical possibilities in the treatment of anaemia. These findings have been published in the journal Blood.
Anaemia is a disease in which the number of red blood cells – or the haemoglobin levels of the red blood cells – is lower than normal. A major factor in the morbidity and mortality of one third of the world’s population, anaemia is a major public health problem.
Anaemia can be caused by a deficit of iron in the blood resulting from dietary deficiencies, infections, chronic diseases, heavy menstruation, problems during pregnancy or by genetic diseases that affect the production of red blood cells (thalassaemia).
An essential component of the haemoglobin in red blood cells, iron is crucial to many biological processes – including the transport and storage of oxygen in the body. In other words, insufficient iron in the body means insufficient haemoglobin and red blood cells for transporting oxygen to the organs and tissues, which ultimately leads to organ failure.
For more information: C’est quoi l’hémoglobine ? (only available in French)
However, too much iron is also toxic to the body, meaning that its intake needs to be carefully regulated to avoid excessively high or low levels which are responsible for severe clinical complications.
Understanding iron metabolism
For several years, knowledge about anaemia and iron metabolism has been steadily increasing. It is now well known that iron levels in the body are regulated by a hormone called hepcidin.
We also now know that if the body needs more iron, as is the case with anaemia, a hormone called erythroferrone (ERFE) suppresses the expression of hepcidin in the liver. This process supplies the bone marrow with iron to synthesise new red blood cells and increase haemoglobin levels.
The identification of ERFE in 2014 by Inserm researcher Léon Kautz and his colleagues represented an important step in this field of research. However, these data obtained ten years ago were already suggesting that ERFE was not the only hormone controlling this process. The scientists hypothesised that a second protein, previously unknown, performed a similar function.
A new factor identified
This is what they have now confirmed by conducting new experiments in mouse models of anaemia, in two specific cases: one during an increased synthesis of red blood cells aimed at correcting induced anaemia in mice and the other in mice with thalassaemia.
The scientists started by studying the molecular mechanisms activated in the animals’ liver to identify the genes whose expression was increased during the anaemia. They observed that the expression of the gene coding for protein FGL1 was increased in the liver when the oxygen concentration decreased.
The researchers then produced different forms of protein FGL1 to test its mode of action in vivo in mice and in vitro in human liver cells. They were able to show that its mode of action is similar to that of the hormone ERFE, because FGL1 also represses hepcidin expression.
‘In addition to the fundamental aspects of this research in understanding anaemia, we believe that identifying the role of FGL1 will lead to the development of new therapeutic strategies to treat anaemia of various causes and for which the current treatments are ineffective,’ emphasises Léon Kautz, Inserm staff scientist.
For the moment, the team will start by conducting additional research to verify that FGL1 levels are indeed increased in the blood of patients with different types of anaemia. But the scientists plan to go further, with Inserm Transfert having already filed two patent applications for this study.
On the one hand, the first patent aims to better treat anaemia resulting from chronic diseases such as cancer. The objective is to identify analogous molecules or molecules that activate FGL1 synthesis, which would reduce hepcidin expression in these patients and increase their haemoglobin levels.
On the other hand, thalassaemia is characterised by very low levels of hepcidin, leading to excess iron that is harmful to the organs, causing high mortality. The team hypothesised that FGL1 is also involved in this process. The second patent therefore aims to achieve proof of concept that FGL1 inhibition could improve iron overloads in patients suffering from thalassaemia.
Léon Kautz
Inserm staff scientist
Unit 1220 Inserm/INRAE/ENVT/Université Toulouse III – Paul-Sabatier, Digestive Health Research Institute
Email: yrba.xnhgm@vafrez.se
Telephone number available on request
The hepatokine FGL1 regulates hepcidin and iron metabolism during anemia in mice by antagonizing BMP signaling
Blood, December 2024
DOI: https://doi.org/10.1182/blood.2023022724
Ugo Sardo,1,* Prunelle Perrier,1,* Kevin Cormier,1 Manon Sotin,1 Jean Personnaz,1 Thanina Medjbeur,1 Aurore Desquesnes,1 Lisa Cannizzo,1 Marc Ruiz-Martinez,2 Julie Thevenin,1 Benjamin Billoré,1 Grace Jung,3 Elise Abboud,4,5 Carole Peyssonnaux,4,5 Elizabeta Nemeth,3 Yelena Z. Ginzburg,2 Tomas Ganz,3,6 and Léon Kautz1
1 Institut de Recherche en Santé Digestive, Université de Toulouse, Inserm, INRAE, ENVT, Université Toulouse III – Paul-Sabatier, Toulouse, France;
2 Icahn Schoolof Medicine Mount Sinai Hospital, New York, NY;
3 Department of Medicine, David Geffen School of Medicine at UCLA, Los Angeles, CA; 4 Institut Cochin, Inserm, Centre National de la Recherche Scientifique, Université de Paris, Paris, France;
5 Laboratory of Excellence GR-Ex, Paris, France;
6Department of Pathology, David Geffen School of Medicine at UCLA, Los Angeles, CA