RVF is transmitted from livestock to humans. © DAAF 976
A viral disease responsible for major epidemics, occurring mainly in Africa, Rift Valley fever (RVF) is transmitted from livestock to humans. Despite being listed as a priority emerging disease by the World Health Organization (WHO) R&D Blueprint program in 2015, there had until now been little research into the dynamics of its transmission. As part of a multidisciplinary collaboration, researchers and public health professionals from Inserm, the French Public Health Agency, Cirad and the London School of Hygiene and Tropical Medicine, with the support of the REACTing consortium, have developed a mathematical model to study the dynamics of the 2018-2019 RVF epidemic in Mayotte and to quantify for the first time the beneficial impact of vaccinating livestock. This research has been published in the journal PNAS.
Against the background of the continued Covid-19 pandemic, research into emerging diseases and zoonoses – infectious diseases transmissible from animals to humans, has never been so important.
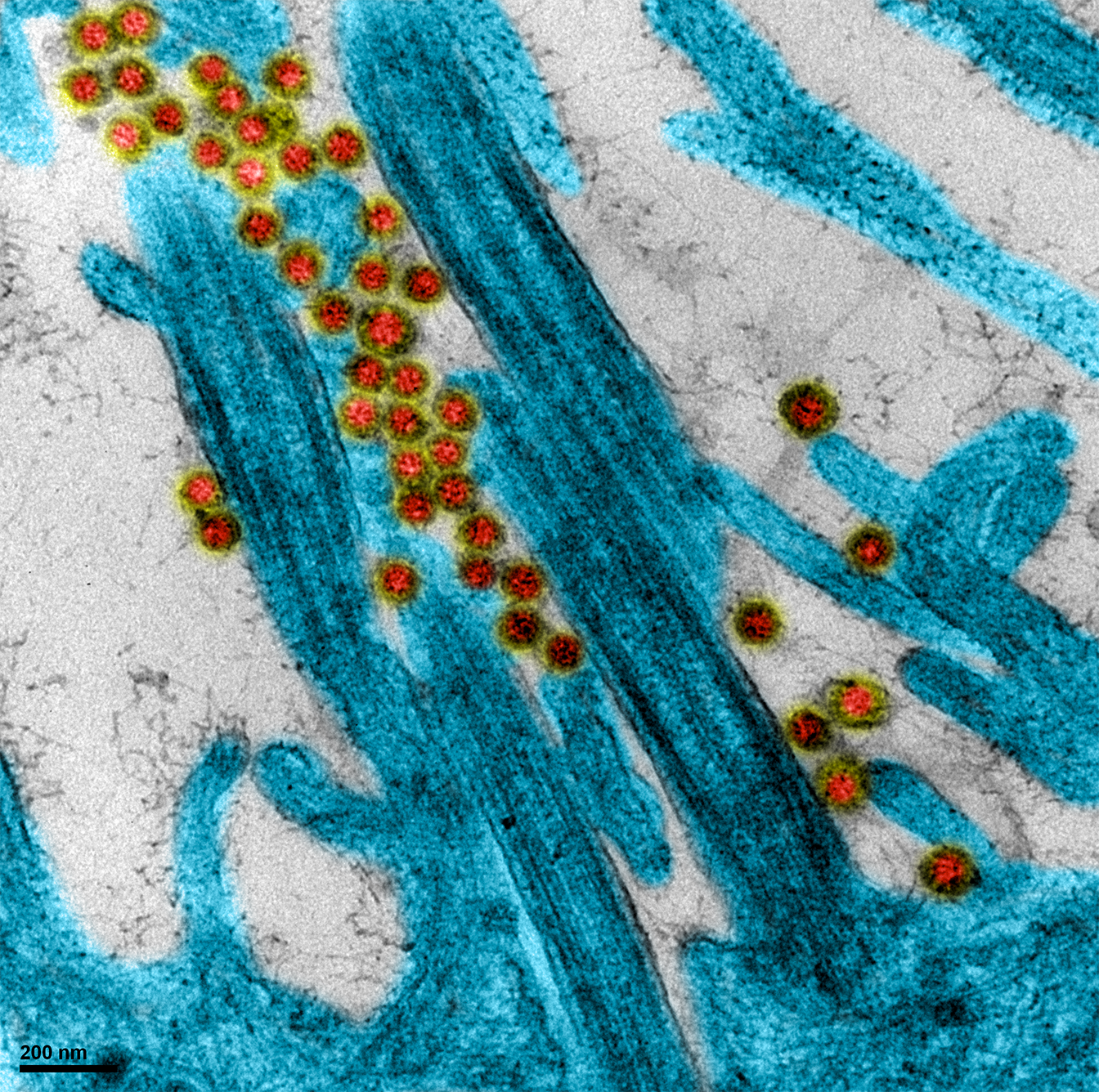
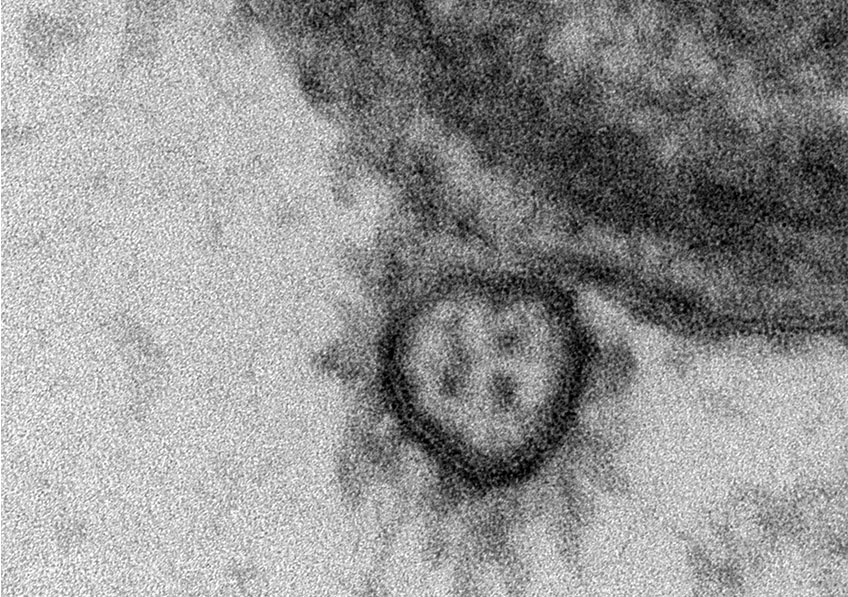
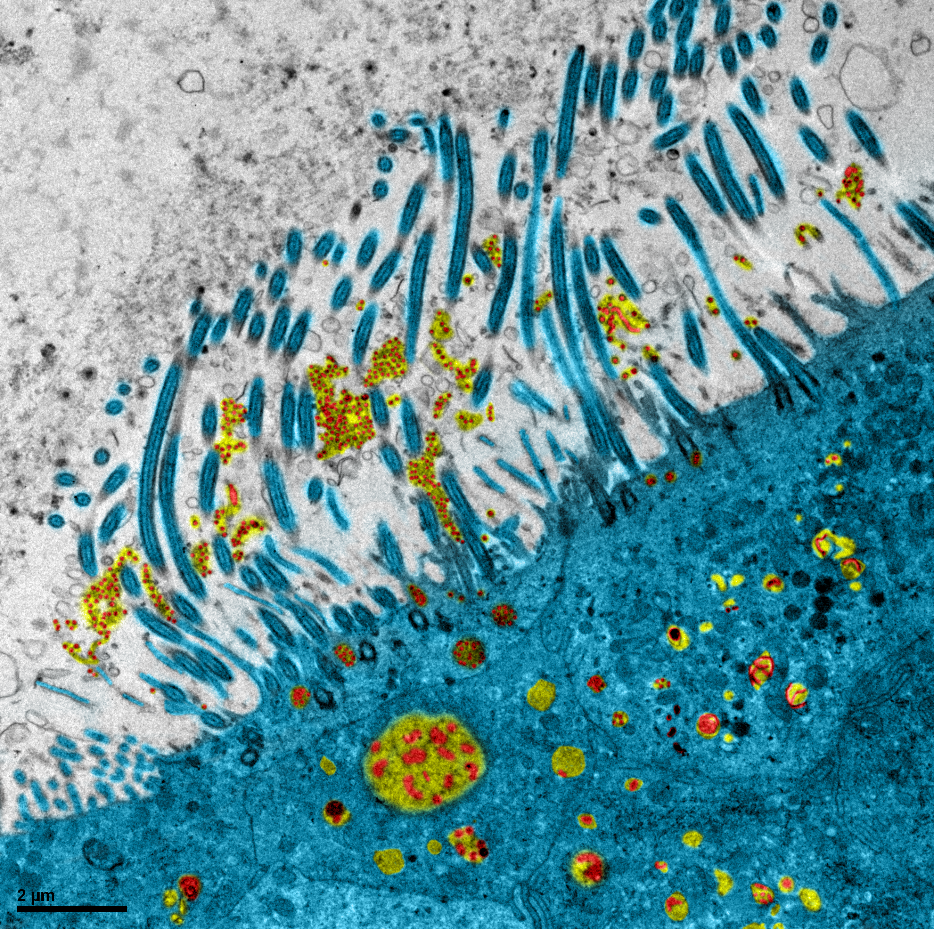
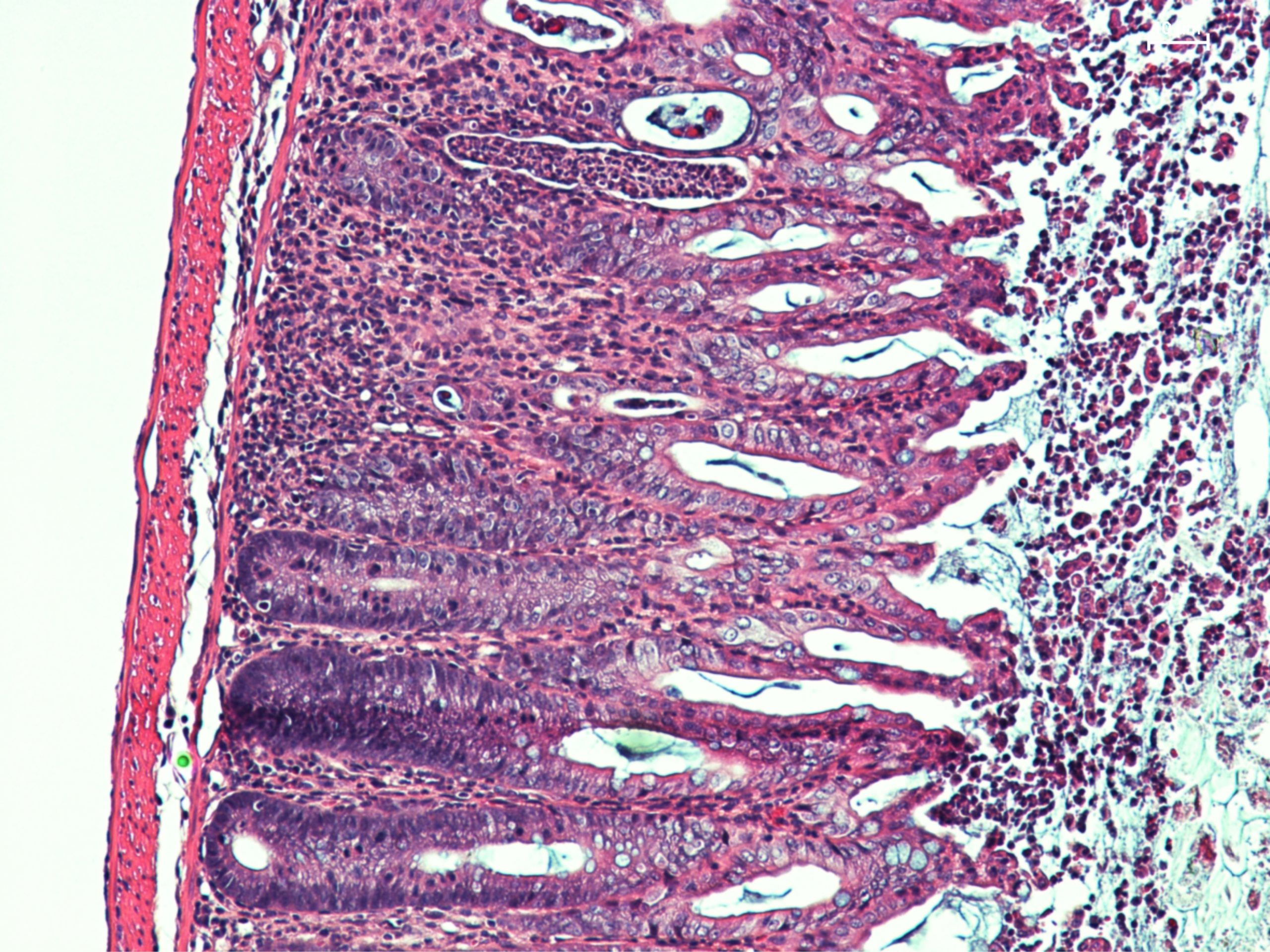
Rift Valley fever (RVF) is a viral zoonotic disease occurring primarily in some African regions, Mayotte and the Arabian Peninsula. It mainly affects livestock, causing waves of miscarriage and widespread mortality in the youngest animals. Humans can be infected through direct contact with the body fluids of contaminated animals or through the bites of infected mosquitos. To date, no human-to-human contamination has been reported. While the majority of patients develop asymptomatic or benign forms, in rare cases (1 to 3% of patients) the disease can take a more severe turn, characterized by ocular and meningeal disorders, and life-threatening hemorrhagic fever.
A major public health concern in some countries, RVF was listed by the WHO as an emerging priority disease in 2015, involving the accelerated development of its means of control. While research into vaccines for livestock is making progress, the potential impact of vaccination on the dynamics of the epidemic had never previously been evaluated.
The team, coordinated by Inserm researcher Raphaëlle Métras and her French Public Health Agency colleague Marion Subiros, looked at the 2018-2019 RVF epidemic in Mayotte. Since 2008, thanks to the implementation of two surveillance systems – one concerning the animals (helped by the Veterinary Services of Mayotte), the other humans – a large amount of high-quality RVF surveillance data has been collected. These data concern livestock seroprevalence and human epidemiology (number of human cases, sociodemographic characteristics, disease exposure criteria and geolocation).
As part of their study, the researchers and their colleagues developed a mathematical model integrating these data collected jointly by the two systems in order to reproduce the transmission dynamic of the virus during the 2018-2019 epidemic. One of the objectives was to obtain more information on how the virus passes from infected animals to humans.
What the scientists have shown is that for the first time in the context of an RVF epidemic there was a higher level of transmission to humans from mosquitos than through direct contact with infected livestock. If it is assumed that 30% of the population of Mayotte are farmers, up to 55% of human infections would have been caused by mosquito bites, versus 45% through exposure to livestock.
This is the first study to provide figures on the distribution of transmission through mosquito bites versus transmission through human direct contact.The team also modeled the potential impact of vaccinating livestock to reduce the scale of the epidemic, using a suitable vaccine with the target characteristics of the WHO Blueprint program (especially vaccine efficacy). The findings of the model show that vaccinating 20% of the livestock could reduce the number of human cases by 30%. Reactive and mass vaccination campaigns in livestock would therefore be an essential measure when it comes to reducing the incidence of the disease in humans.
In a context in which zoonotic disease epidemics are emerging in succession, this research illustrates the importance of implementing a “One Health” approach, taking a systemic and unified approach to public, animal and environmental health at local, national and global levels.“The health emergency associated with the Covid-19 pandemic must force us to rethink how we see the links between human, animal and environmental health. Our research highlights the importance and added value of a multidisciplinary and integrated One Health quantitative approach in fighting zoonotic diseases. They also provide avenues for improving the surveillance of and research into emerging infectious diseases,” concludes Métras.