Researcher Contact
Sandrine Sarrazin
Inserm researcher
Stem cell and macrophage biology team
Jean-Pierre Gorvel
CNRS Research Director
Immunology and cell biology of pathogen/host cell interactions team
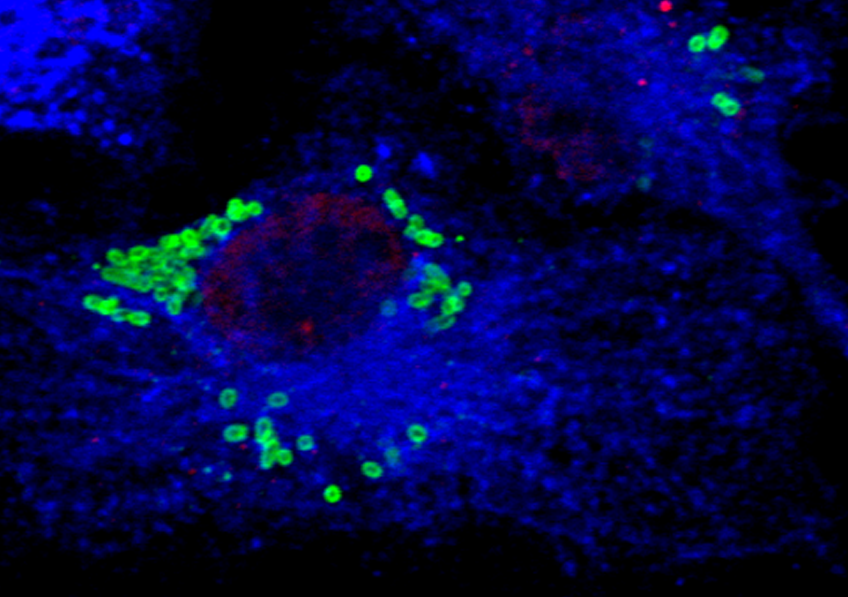 Immune system cell infected with Brucella (green); endocytosis compartment (blue). © CIML
Immune system cell infected with Brucella (green); endocytosis compartment (blue). © CIML
Correct immune system function depends on the continuous supply of white blood cells derived from stem cells that reside in the bone marrow. These are known as blood stem cells or hematopoietic stem cells. Researchers from Inserm, CNRS and Université d’Aix-Marseille at the Center of Immunology Marseille-Luminy have now discovered a new role played by these cells in immune response. In their article published in Journal of Experimental Medicine, they describe how they are able to recognize and directly interact with a bacterium called Brucella in the bone marrow, thanks to a receptor present on their surface. This is the first demonstration of the direct recognition of a living pathogen by the blood stem cells, which attests to their very early contribution to the immune response.
Blood stem cells, otherwise known as hematopoietic stem cells, are stem cells that reside in the bone marrow. They multiply and give rise to all blood cells, namely the red cells that transport oxygen and the white cells that participate in the immune response.
With regard to immune response, the blood stem cells had until now only been seen as the cells from which the white cells originate. However, a growing body of evidence suggests that they can also contribute directly and actively to the immune response. For example, recent data have shown that they can directly detect cytokines, which are proteins released during infection or inflammation.
In a new publication, a research team from Inserm, CNRS and Université d’Aix-Marseille led by Michael Sieweke and Jean-Pierre Gorvel[1] wanted to further the scientific knowledge in this area. The researchers succeeded in describing the mechanisms at work during the encounter between the blood stem cell and a specific pathogen: the Brucella bacterium, which is a mandatory reportable microorganism/toxin (MOT)[2].
Brucella causes an infectious disease called brucellosis (also known as Malta fever or Mediterranean fever), which is one of the most widespread zoonoses posing a significant threat to human health worldwide[3]. Brucella is an intriguing pathogen and very interesting for the scientists to study because of its ability to establish persistent and chronic infections and evade the immune response of its host[4].
The scientists found that the blood stem cells present in the bone marrow were able to detect Brucella. Their observations show that CD150, a specific receptor on the surface of the blood stem cells, interacts with Omp25, a protein present on the surface of Brucella.
 Graphic Summary of the Discovery. Thanks to the CD150 receptor on their surface, the blood stem cells in the bone marrow are able to detect Brucella. After recognizing it, they begin to produce more white blood cells. © CIML
Graphic Summary of the Discovery. Thanks to the CD150 receptor on their surface, the blood stem cells in the bone marrow are able to detect Brucella. After recognizing it, they begin to produce more white blood cells. © CIML
“Our study reveals the mechanisms by which these blood cells are able to detect bacteria via a special receptor. We can consider this as a direct ‘handshake’ between the stem cell and the bacterium. Never had anyone imagined that the blood stem cell could recognize a living bacterium,” explains Sandrine Sarrazin, Inserm researcher and co-last author of the study.
The scientists then showed that this “handshake” leads to a rapid response by the stem cells, whereby they begin to produce more white blood cells. This is the first demonstration of the direct recognition of a living pathogen by blood stem cells and attests to a very early and unexpected contribution of these cells to the immune response.
How Brucella Uses Stem Cells to “Hack” the Immune System
The scientists then wondered whether this mechanism was more beneficial to the host or to the bacterium.
Thanks to meticulous observations, they found that Brucella directs the stem cells to produce the white blood cells it favors for infection. The bacterium is able to invade the white blood cells produced by the blood stem cells and use them to multiply and establish itself in the body. In this particular case, the stem cells therefore contribute to the spread of the bacterium.
“This research sheds new light on the sophisticated mechanisms that pathogens use to evade the immune system’s defenses. While the increased production of white blood cells would be beneficial if they could effectively fight infection, Brucella is able to exploit them in order to multiply,” explains Gorvel, one of the co-last authors of the study.
“This mechanism can be seen as an evasion strategy used by the bacterium to advance the infection,” summarizes Sieweke, another co-last author of the study.
The publication of this study marks an important step in understanding the complex dance between Brucella and the hematopoietic stem cells. It not only provides crucial information on the pathogenesis of brucellosis, but also opens up new avenues for the development of targeted therapeutic interventions.
“In addition to improving knowledge about how the immune response works, our study ultimately allows us to envisage the development of a targeted therapy capable of preventing the interactions between Brucella and the blood stem cell, preventing the spread of the bacteria in the body and helping patients with brucellosis,” concludes Gorvel.
[1] This research is the result of a collaboration between two research teams at the Center of Immunology Marseille-Luminy (CIML, CNRS/Inserm/Aix-Marseille Université): Michael Sieweke’s Stem cell and macrophage biology team and Jean-Pierre Gorvel’s Immunology and cell biology of pathogen/host cell interactions team.
[2] The Brucella experiment was therefore conducted at the Center for Immunophenomics (CIPHE) under biosafety level 3 conditions.
[3] The World Health Organization (WHO) has identified brucellosis as being one of the seven most neglected zoonoses, contributing to poverty, hindering development, and causing substantial economic losses in developing countries.
[4] Previous studies conducted at Gorvel’s laboratory had enabled crucial discoveries with the aim of elucidating the mechanisms underlying these phenomena.
Sandrine Sarrazin
Inserm researcher
Stem cell and macrophage biology team
Jean-Pierre Gorvel
CNRS Research Director
Immunology and cell biology of pathogen/host cell interactions team
CD150-dependent hematopoietic stem cell sensing of Brucella instructs myeloid commitment
Lisiena Hysenaj1,2, Bérengère de Laval1, Vilma Arce-Gorvel1, Mile Bosilkovski, Gabriela González-Espinoza1, Guilhaume Debroas1, Michael H. Sieweke1,4, Sandrine Sarrazin and Jean-Pierre Gorvel
1 Aix Marseille University, Centre National de la Recherche Scientifique, Institut National de la Santé et de la Recherche Médicale, Centre d’Immunologie de Marseille-Luminy, Marseille, France
2 Department of Anatomy, University of California, San Francisco, San Francisco, CA, USA
3 University Clinic for Infectious Diseases and Febrile Conditions, Skopje, Republic of North Macedonia
4 Center for Regenerative Therapies Dresden, Technische Universität Dresden, Dresden, Germany
Journal of Experimental Medicine, avril 2023