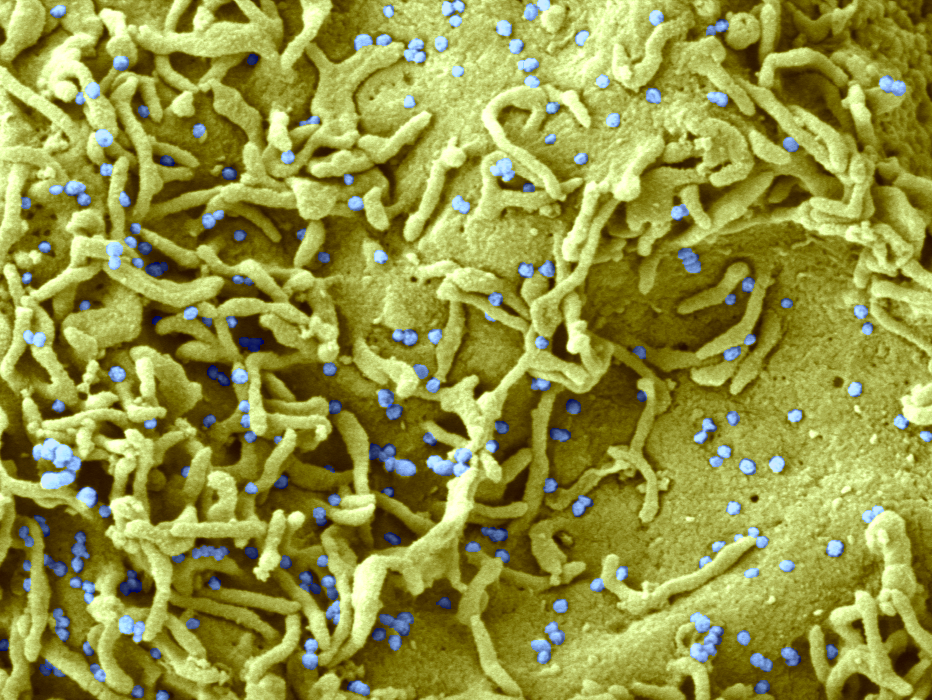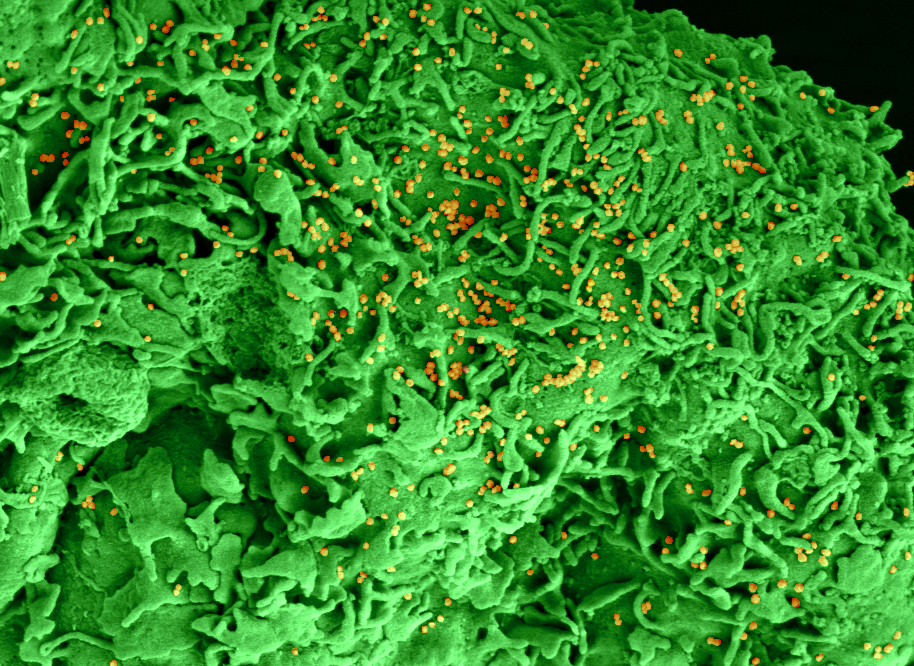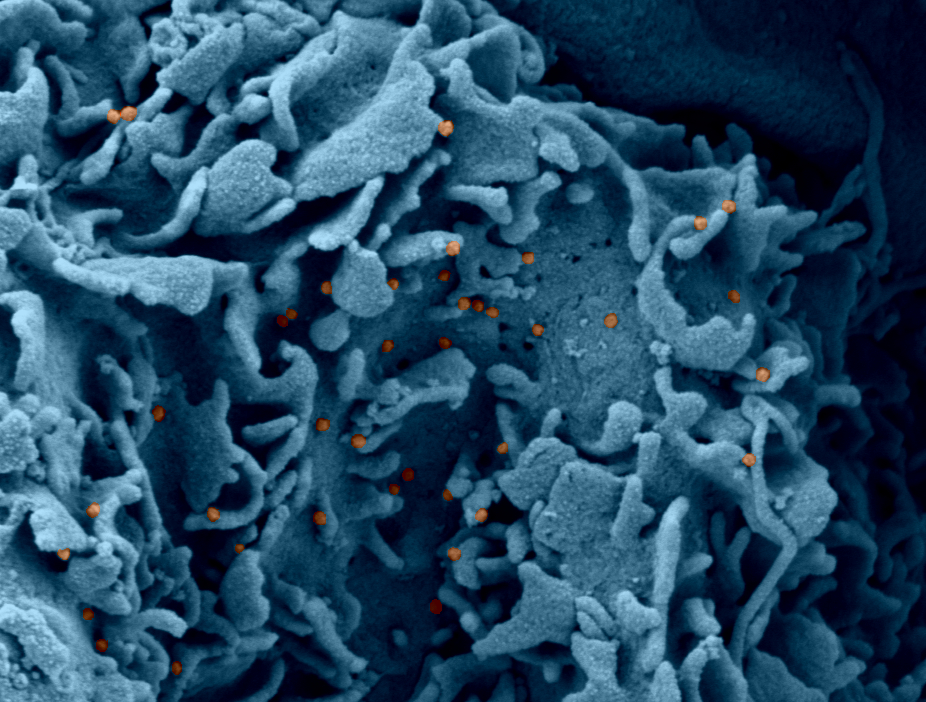
@ NIAID
Researchers from the ComPaRe cohort (Community of Patients for Research, compare.aphp.fr ), led by Prof. Philippe Ravaud, AP-HP / University of Paris / Inserm, used an original method to develop and validate the first measurement science of the severity of the disease and its impact on the lives of patients. This study involving 1,022 patients suffering from long Covid was published in the journal Clinical Infectious Diseases on April 29, 2021.
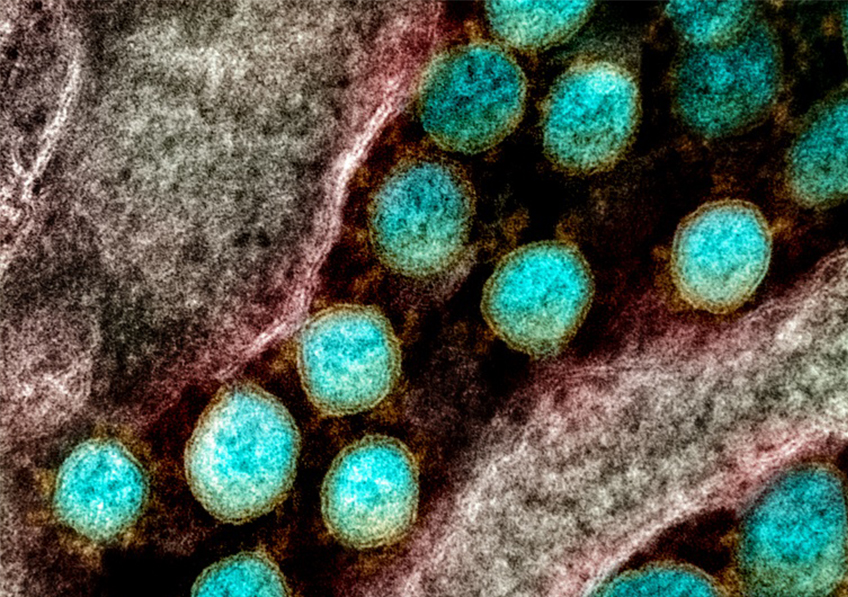
“Long covid” is the term used by patients to describe the set of late manifestations occurring after infection with the SARS-CoV-2 virus. According to the National Statistics Office in the UK, around one in 10 infected people continue to have symptoms 12 weeks after the onset of infection. There are many causes for the persistence of symptoms. For example, there are organ sequelae following the acute phase of the disease (pulmonary scars, complications of resuscitation, etc.), post-traumatic stress linked to the disease or its management, viral persistence or post-viral fatigue syndrome. In a given individual, several causes are often intertwined and responsible for complex clinical pictures.
Until now, scientific studies estimating the number of patients with persistent symptoms of Covid have each used a different definition of the disease. The heterogeneity of the measures used may therefore have contributed to the discrepancies between the results of the studies.
To respond to this problem, the clinical epidemiology center of the Hôtel-Dieu AP-HP hospital, headed by Prof. Philippe Ravaud, AP-HP / University of Paris / Inserm, launched a study at the end of 2020 on the long Covid within the ComPaRe cohort, the Community of Patients for Research supported by Public Assistance – Hospitals of Paris and University of Paris. This study aimed to develop a scientific measure of the severity of the disease and its impact on the lives of patients using a two-phase method.
During the first phase (October – November 2020), the researchers interviewed 492 patients [median age 45 years, 84% female, 43% with infection confirmed by PCR] with a long covid (defined as the presence of persistent symptoms at least 3 weeks after infection with SARS CoV2). Patients were able to report, in free text, all of their symptoms and the triggers and calming factors thereof. Patients were also asked about the impact of the disease on their lives. The participants’ responses were analyzed by researchers and expert patients. They allowed the definition of a list of 53 manifestations of the disease (fatigue, chest pain, headaches, balance disorders, etc.) and six areas of patients’ lives that could be impacted by it. ci (family life,
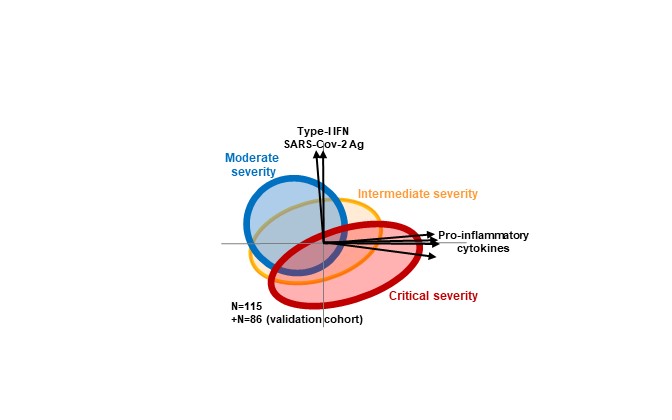
In the second phase (November 2020 – February 2021), the researchers used these results to develop a questionnaire, completed directly by the patients, in order to measure the severity of the disease and its impact on the patients’ lives. They assessed the validity, reliability and relevance of this questionnaire in a second sample of 1022 patients with a long Covid [median age 45 years, 79% of women, 55% of patients with an infection confirmed by PCR, 12% with been hospitalized]. This second phase showed the major impact of long covid on the quality of life of patients, estimated to be around 40% lower than that of the general population. So,
In conclusion, this research has enabled the development of a quality scientific basis for measuring long covid. Standardization of measurements in scientific studies will make it possible to compare and combine the results thereof.
The measure developed is currently used to assess the evolution over time of the symptoms of patients in the ComPaRe Covid long study. This will make it possible to understand the variations in the manifestations of the disease over time and to answer the question “how long does the disease last?” “.
In order to answer these research questions, ComPaRe renews its call for participation in long-term Covid research projects carried out within the cohort. To participate, simply register on https://compare.aphp.fr .
Created in 2017 by the AP-HP, ComPaRe, the Community of Patients for Research today brings together more than 45,000 patient volunteers across France. They help advance research on their chronic disease (s) by regularly responding to researchers’ online questionnaires, on the secure platform https://compare.aphp.fr .
Today, 36 specific projects have been launched in ComPaRe. In addition to the long covid, several specific studies have been launched to follow patients suffering from diabetes, Verneuil’s disease, vitiligo, chronic low back pain, kidney disease, vasculitis, high blood pressure, endometriosis, neurofibromatosis and of Marfan syndrome. New studies and specific cohorts are being set up.