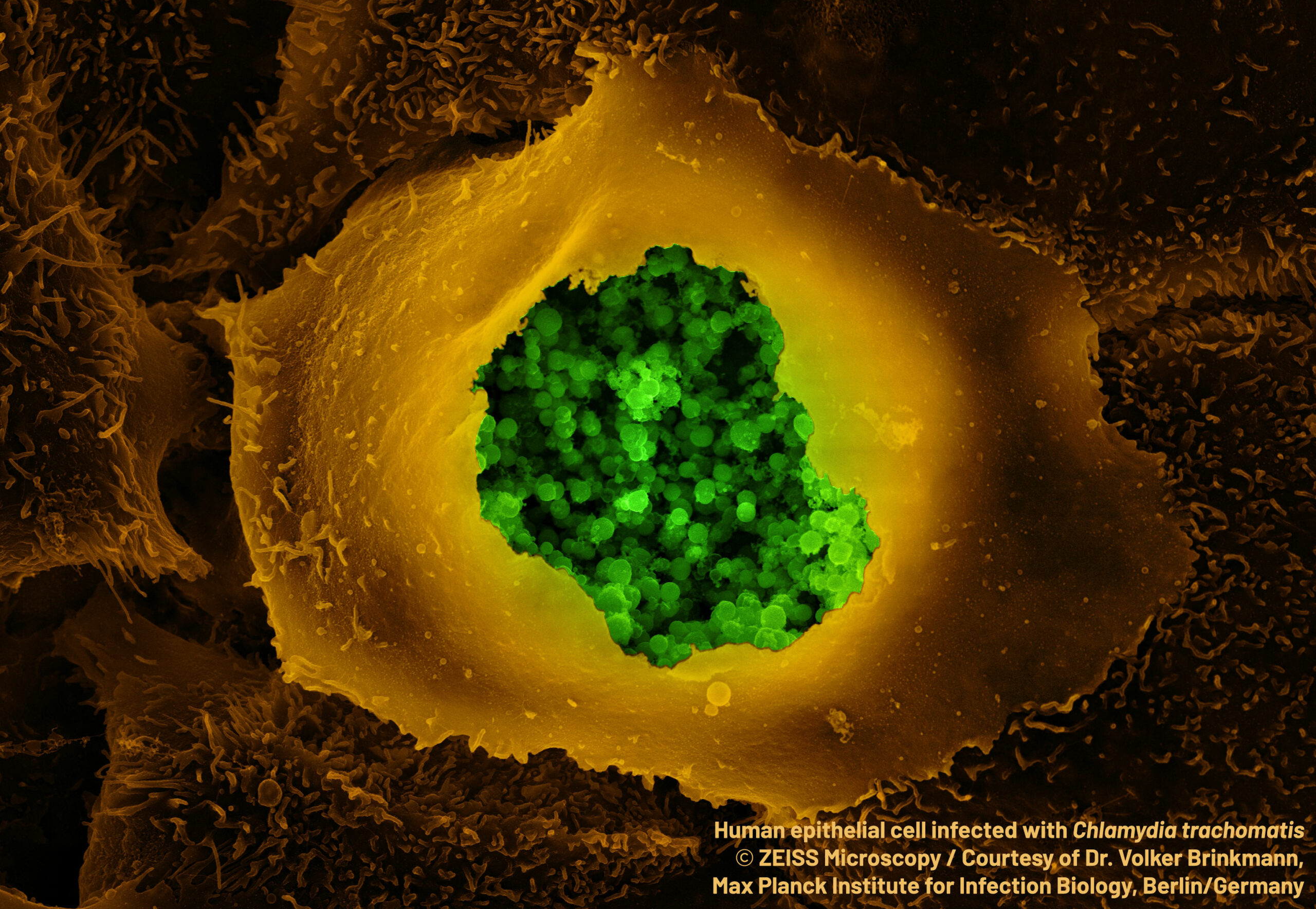
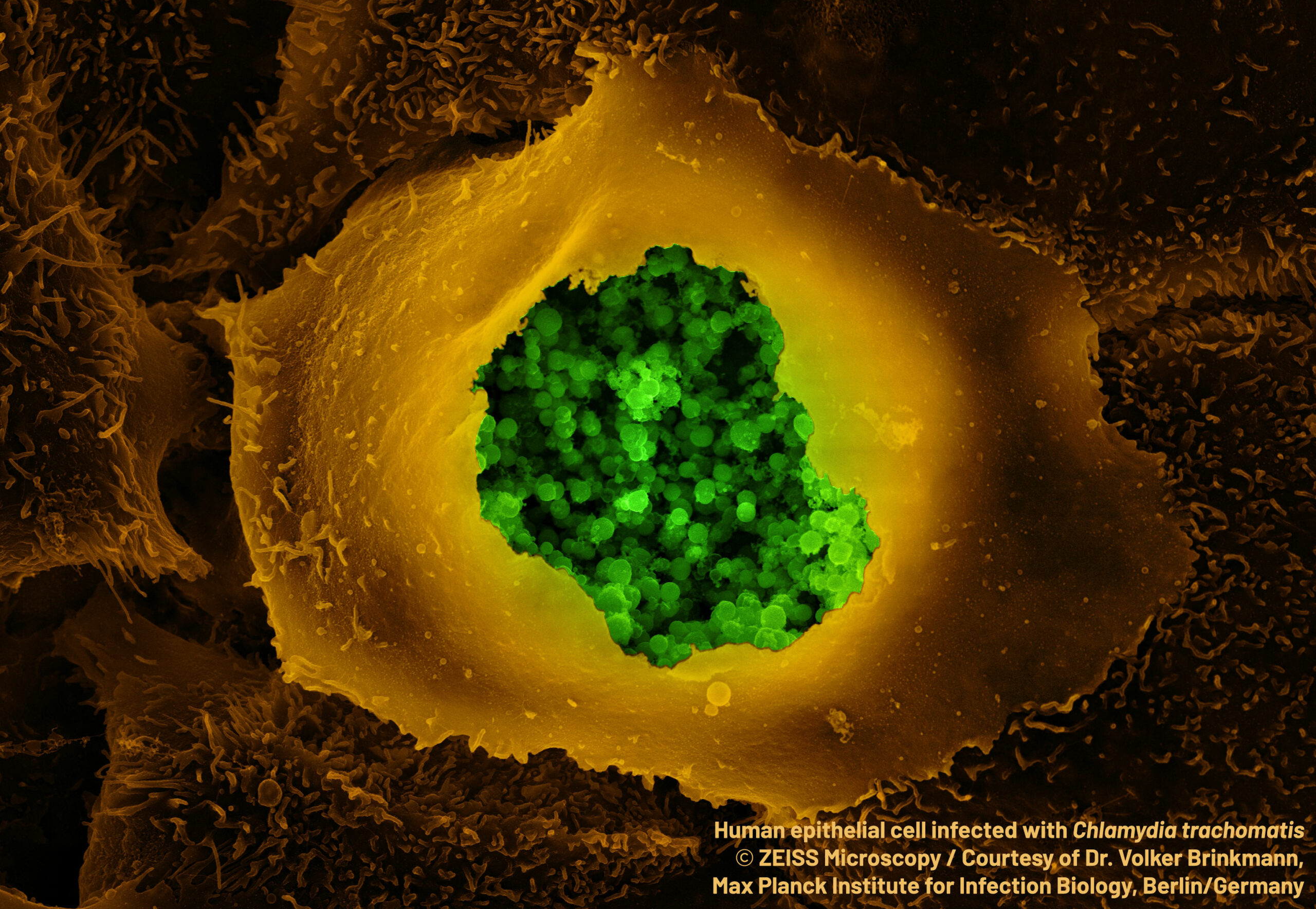
Chlordecone is an organochlorine insecticide that was used in the French West Indies from 1973 to 1993 to control the banana root borer. © Adobe Stock
Despite the fact that chlordecone has not been used as an insecticide in the French West Indies for 30 years now, its persistence in the environment continues to contaminate the populations. While its neurotoxic properties are well established, its impact on neurodevelopment remains to be clarified. An international research team involving Inserm researchers at the Research Institute for Environmental and Occupational Health (Inserm/Université de Rennes/EHESP School of Public Health) studied the impact of pre- and postnatal chlordecone exposure on the cognitive and behavioral abilities at 7 years of age of 576 children from the TIMOUN mother-child cohort in Guadeloupe[1]. Their research shows that this exposure is associated with poorer scores on tests evaluating cognitive abilities and behavioral disorders, with the impact differing according to the child’s sex. These results, published in Environmental Health, call for consideration to be given to the potential impact of these effects at population level, in order to optimize prevention policies.
Chlordecone is an organochlorine insecticide that was used in the French West Indies from 1973 to 1993 to control the banana root borer. Its persistence in the environment is responsible for contaminating the population through the consumption of contaminated foodstuffs. Chlordecone is now considered to be neurotoxic, toxic to reproduction and development, carcinogenic, and an endocrine disruptor. Experimental studies in animals have also shown that exposure of females to chlordecone during gestation leads to neurobehavioral and learning disorders in the offspring, the nature and intensity of which varies according to sex.
The neurotoxicity of chlordecone can be explained by its ability to interact with numerous neurotransmitters[2] and by its hormonal properties, particularly its action on estrogens. Yet estrogens play a crucial role, which differs according to chromosomal sex, in the development of the brain.
In the face of these observations, and in order to better estimate the potential impact of pre- and postnatal exposure to chlordecone on child neurodevelopment, Inserm researchers from the Research Institute for Environmental and Occupational Health (Inserm/Université de Rennes/EHESP School of Public Health), as part of an international research team, examined the intellectual abilities and behaviors of 576 children from the TIMOUN mother-child cohort in Guadeloupe.
In order to assess the children’s levels of pre- and postnatal exposure to chlordecone, the concentration of the pesticide was measured in umbilical cord blood at birth and in the blood of the children at 7 years of age. Their intellectual abilities were assessed according to 4 criteria: verbal comprehension, information processing speed, working memory[3], and perceptive reasoning[4].
The mothers also completed a questionnaire to measure the presence of behavioral difficulties in their child which can be categorized as either “internalizing” – in the form of emotional symptoms and interpersonal problems with peers, or “externalizing” – in the form of social behavior problems (anger, defiance, etc.), hyperactivity, and/or inattention.
Prenatal exposure to chlordecone was found to be associated, for each doubling of the level of exposure, with a 3% increase in the score estimating “internalizing” behavioral difficulties at 7 years of age, with a stronger association among girls (+7%) than among boys (0%).
Postnatal chlordecone exposure was found to be associated with poorer scores estimating general intellectual abilities (0.64 IQ point decrease for each doubling of the level of exposure). This manifests, particularly in boys, as a decrease in perceptive reasoning, working memory and verbal comprehension. In addition, postnatal exposure was associated with a greater number of “externalizing” behavioral difficulties in both boys and girls.
These findings indicate that exposure to chlordecone during periods of in utero development or during childhood is associated with a reduction in intellectual abilities and an increase in behavioral difficulties, with effects sometimes differing in nature and intensity according to sex.
“This is consistent with the estrogenic properties of this pesticide and its effects that vary according to sex and period of brain development,” explains Luc Multigner, Inserm research director who participated in this research.
According to the research team, it is therefore justified to pursue public policies aimed at reducing exposure to chlordecone, particularly among the most vulnerable populations, such as children and pregnant women. The team also calls for monitoring of the prevalence and management of children presenting with psychomotor retardation, sensory, neuromotor or intellectual disorders and/or interpersonal difficulties.
“Although the neurological and neurobehavioral effects observed in this study are relatively moderate and subtle at the individual level, they may, given the widespread exposure of the French West Indian population to chlordecone, have a non-negligible impact at the population level,” concludes Multigner.
[1] The TIMOUN mother-child cohort was designed to evaluate the health impact of chlordecone exposures on pregnancy and childhood development. Led by the Research Institute for Environmental and Occupational Health (Inserm/Université de Rennes/EHESP School of Public Health) and the Gynecology-Obstetrics Department of University Hospital Guadeloupe, this cohort consists of 1,068 women included during their pregnancy between 2004 and 2007. Following their birth, the children were monitored at 3, 7 and 18 months of age and then at 7 years of age.
[2] Neurotransmitters are chemical substances that ensure the transmission of information between nerve cells.
[3] Working memory is a form of short-term memory that uses the information obtained in the present moment in the performance of a specific task.
[4] Perceptive reasoning measures the cognitive ability to integrate and manipulate visual and spatial information in order to solve complex visual problems.



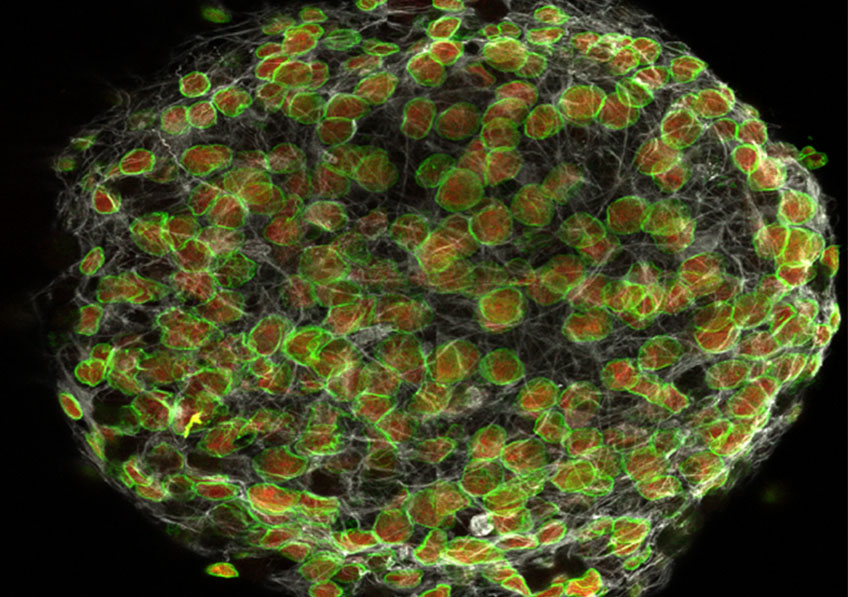


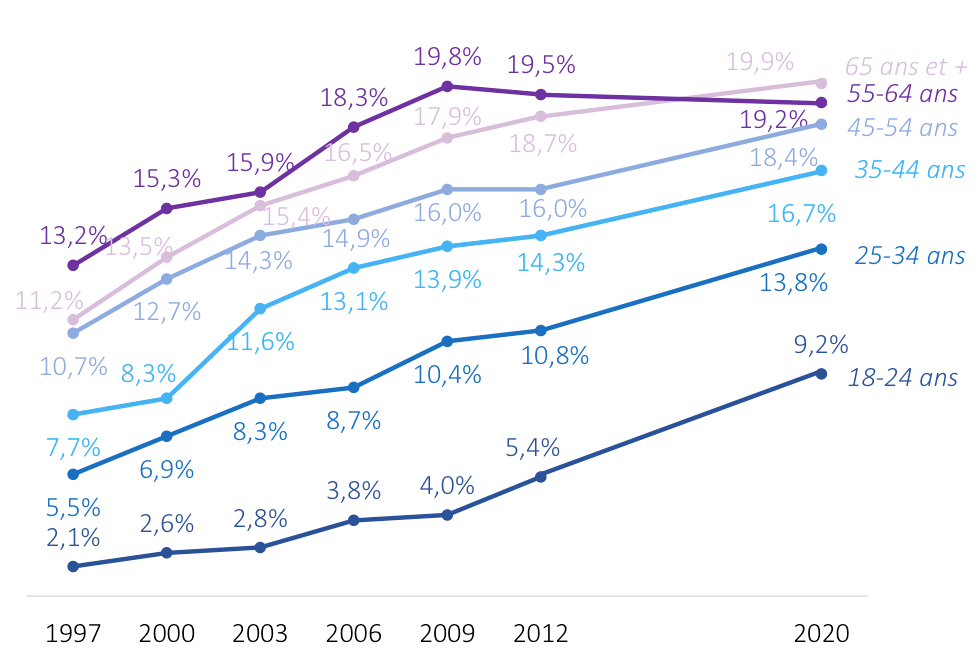 Evolution of the prevalence of obesity by age groups between the 1997-2012 Obépi-Roche surveys and the 2020 Obépi survey.
Evolution of the prevalence of obesity by age groups between the 1997-2012 Obépi-Roche surveys and the 2020 Obépi survey.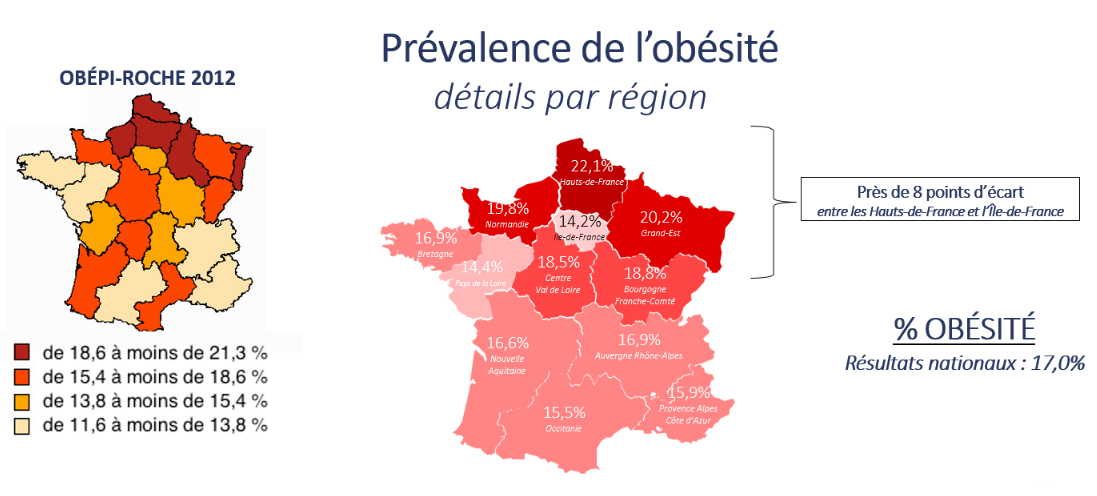 Geographic distribution of the prevalence of obesity in 2020 in the French regions
Geographic distribution of the prevalence of obesity in 2020 in the French regions