Researcher Contact
Nicolas Venteclef
Inserm researcher
Necker Enfants Malades Institute (Inserm/Université Paris Cité/CNRS)
E-mail: avpbynf.iragrpyrs@vafrez.se
Telephone number available on request
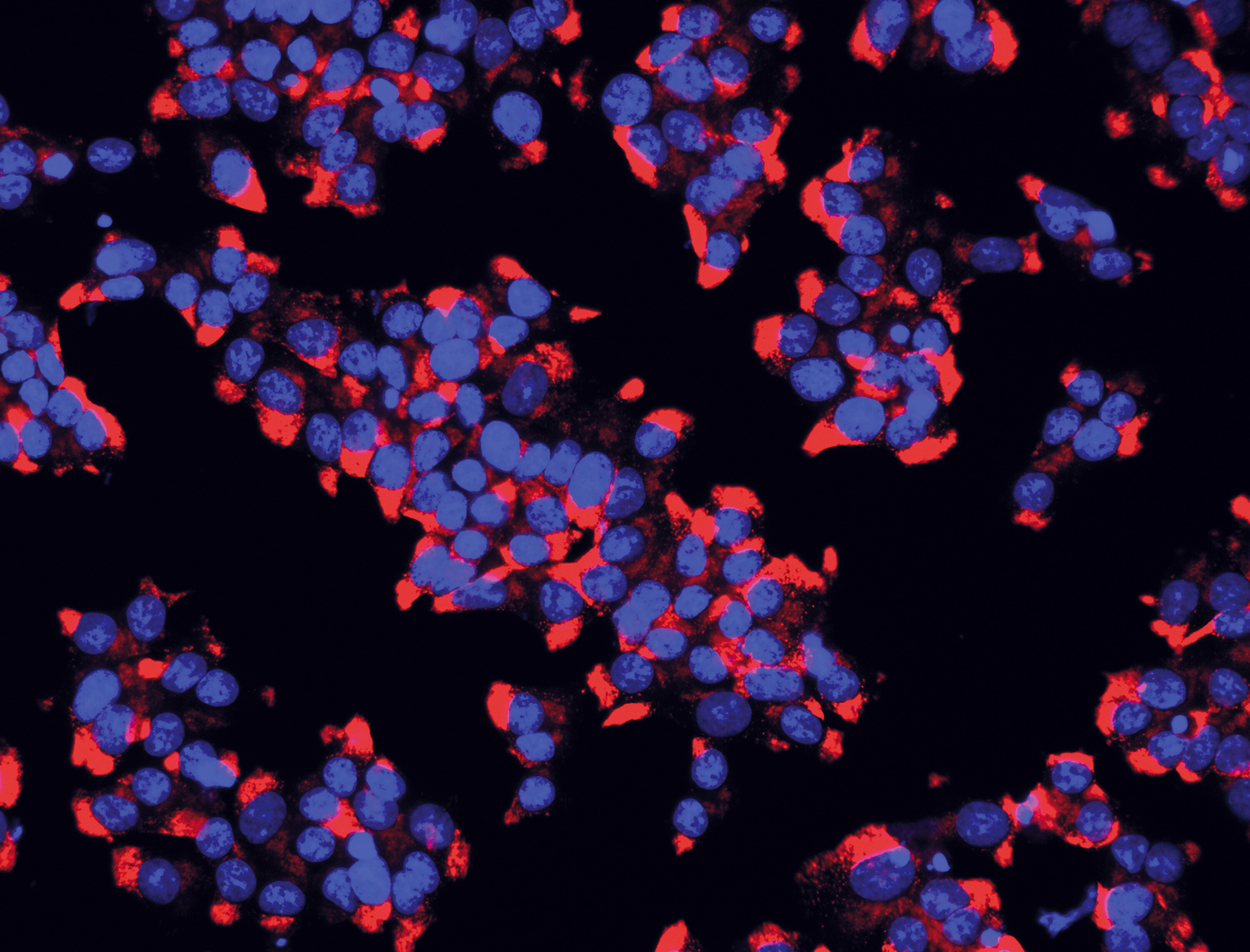 Image taken from the January-February 2013 issue of Science & Santé magazine, Special Feature, page 30. Human pancreatic beta cells. In blue, the cell nuclei; in red, the insulin contained in the cells.
Image taken from the January-February 2013 issue of Science & Santé magazine, Special Feature, page 30. Human pancreatic beta cells. In blue, the cell nuclei; in red, the insulin contained in the cells.
Scientists from Inserm, Université Paris Cité and CNRS at the Necker Enfants Malades Institute in Paris have identified a new prognostic marker for cardiovascular risk in people with type 2 diabetes (T2D). Led by Inserm researcher Nicolas Venteclef, the team has shown that the number of white blood cells circulating in the blood, as well as certain subtypes, is associated with stroke or myocardial infarction risk over the next ten years. Published in Circulation Research, this finding could make it possible to screen for T2D patients with the highest risk in order to improve prevention. The team filed a patent at the end of 2023 to protect their discovery.
During their lives, people with type 2 diabetes (T2D) have an approximate two-fold higher risk of an atherosclerosis-related cardiovascular event, such as myocardial infarction or stroke, in relation to those without T2D. Atherosclerosis is a disease characterised by the presence of plaques along the wall of the arteries that can rupture and obstruct blood flow.
Identifying those who are most at risk of developing this disease out of the T2D population remains very difficult. The ten-year predictive scores that integrate various cardiovascular risk factors, such as age, smoking and cholesterol levels, are unreliable when applied to this population, including when T2D-specific factors (duration of diabetes, HbA1c glycated haemoglobin, etc.) are taken into account. So it is important to identify new predictive factors for this specific population.
In a new study, the team of Inserm researcher Nicolas Venteclef at the Necker Enfants Malades Institute (Inserm/Université Paris Cité/CNRS) looked at monocytes – a category of white blood cells circulating in the blood, which are directly involved in the onset and progression of atherosclerosis. By evaluating the number of monocytes in the blood and the subtypes present in T2D patients, the researchers wanted to see if these parameters could constitute markers associated with cardiovascular risk.
In atherosclerosis, the blood monocytes are ‘recruited’ in the internal walls of the arteries. There, they differentiate into macrophages, which are cells able to capture ‘bad cholesterol’ and produce inflammatory molecules. The more the macrophages accumulate, the more lipids they capture, increasing the inflammation and the growth of the atherosclerotic plaque. Eventually, these plaques can damage the arterial wall, obstruct the vessel, or rupture.
Three cohorts of patients
The team based their research on three cohorts of T2D patients. Firstly, in AngioSafe-2[1], a cohort including 672 T2D patients, the researchers saw that the circulating monocyte count was positively correlated with the extent of atherosclerotic plaque and thus with the risk of atherosclerosis-related cardiovascular events, regardless of patient age and duration of T2D. In other words, the higher the circulating monocyte count, the greater the risk of a cardiovascular event.
This initial finding was confirmed in a second cohort, GLUTADIAB, comprising 279 people with T2D. This research also included the molecular analysis of circulating monocytes in both cohorts, making it possible to identify certain subtypes of monocytes predominant in T2D subjects with high cardiovascular risk.
What remained to be understood was how the scientists could use this finding to predict cardiovascular risk. A third cohort, SURDIAGENE, which follows people with T2D[2], enabled the authors to obtain the total circulating monocyte counts for 757 patients receiving follow-up in the cardiovascular prevention setting. When correlating these counts with the cases of myocardial infarction or stroke occurring in the cohort, they found that T2D patients with monocyte counts above a certain threshold (0.5 × 109/L) had a five to seven times higher risk of cardiovascular events within ten years compared to those with counts below this threshold.
Armed with these findings, the scientists filed a patent to protect their discovery. They are now working on developing an electronic sensor to measure circulating monocytes from the collection of a drop of blood[3] by classifying them according to subtype. Ultimately, their objective is to include this analysis in the existing prognostic cardiovascular risk scores, in order to identify T2D patients most at risk and improve prevention.
Inserm Transfert has filed a patent for this research.
[1] recruited in the diabetes departments of the Lariboisière and Bichat Claude Bernard AP-HP hospitals
[2] Followed up in the endocrinology department of Nantes University Hospital
[3] in partnership with the PRINT’UP public institute
Nicolas Venteclef
Inserm researcher
Necker Enfants Malades Institute (Inserm/Université Paris Cité/CNRS)
E-mail: avpbynf.iragrpyrs@vafrez.se
Telephone number available on request
Blood Monocyte Phenotype Is A Marker of Cardiovascular Risk in Type 2 Diabetes
Circulation Research, janvier 2024
DOI: 10.1161/CIRCRESAHA.123.322757
Jean-Baptiste Julla # 1 2 3 4, Diane Girard # 1 2 3, Marc Diedisheim 1 2 3 5, Pierre-Jean Saulnier 6, Bao Tran Vuong 1 2 3, Camille Blériot 1 2 3, Elena Carcarino 1 2 3, Joe De Keizer 7, Lucie Orliaguet 1 2 3, Ivan Nemazanyy 1, Charline Potier 1 2 3, Kennan Khider 1 2 3, Dorothy Chepngenoh Tonui 1 2 3, Tina Ejlalmanesh 1 2 3, Raphaelle Ballaire 1 2 3, Hendrick Mambu Mambueni 8, Stéphane Germain 9, Bénédicte Gaborit 10 11, Tiphaine Vidal-Trécan 3 4, Jean-Pierre Riveline 1 2 3 4, Henri-Jean Garchon 8, François Fenaille 12, Sophie Lemoine 13, Aurélie Carlier 14, Florence Castelli 12, Louis Potier 1 2 3 14, David Masson 15 16 17 18, Ronan Roussel 1 2 3 14, Claire Vandiedonck 1 2 3, Samy Hadjadj 7, Fawaz Alzaid 1 2 3 19, Jean-François Gautier 1 2 3 4, Nicolas Venteclef 1 2 3
1 Inserm, Necker Enfants Malades (INEM), Inserm U1151, CNRS UMR 8253, IMMEDIAB Laboratory (J.-B.J., D.G., M.D., B.T.V., C.B., E.C., L.O., I.N., C.P., K.K., D.C.T., T.E., R.B., J.-P.R., L.P., R.R., C.V., F.A., J.-F.G., N.V.), Université Paris Cité, France.
2 Cordeliers Research Centre, Inserm, IMMEDIAB Laboratory, Sorbonne Université (J.-B.J., D.G., M.D., B.T.V., C.B., E.C., L.O., C.P., K.K., D.C.T., T.E., R.B., J.-P.R., L.P., R.R., C.V., F.A., J.-F.G., N.V.), Université Paris Cité, France.
3 Diabetes Institute (J.-B.J., D.G., M.D., B.T.V., C.B., E.C., L.O., C.P., K.K., D.C.T., T.E., R.B., T.V.-T., J.-P.R., L.P., R.R., C.V., F.A., J.-F.G., N.V.), Université Paris Cité, France.
4 Diabetology, Endocrinology and Nutrition Department, Lariboisière Hospital, Fédération de Diabétologie, France (J.-B.J., T.V.-T., J.-P.R., J.-F.G.).
5 Clinique Saint Gatien Alliance (NCT+), Saint-Cyr-sur-Loire, France (M.D.).
6 Poitiers Université, CHU Poitiers, Inserm, Centre d’Investigation Clinique CIC1402, Poitiers, France (P.-J.S.).
7 Nantes Université, CHU Nantes, CNRS, Inserm, l’institut du thorax, Nantes, France (J.D.K., S.H.).
8 Genomics platform UFR Simone Veil 1173; U, University of Versailles Paris-Saclay; Inserm UMR 1173 (H.M.M., H.-J.G.).
9 Center for Interdisciplinary Research in Biology (CIRB), College de France, CNRS, Inserm, Université PSL, Paris, France (S.G.).
10 C2VN, INRAE, Inserm, Aix Marseille University, Marseille, France (B.G.).
11 Department of Endocrinology, Metabolic Diseases and Nutrition, Pôle ENDO, AP-HM, Marseille, France (B.G.).
12 Université Paris-Saclay, CEA, INRAE, Département Médicaments et Technologies pour la Santé (MTS), MetaboHUB, France (F.F., F.C.).
13 Genomics core facility, Institut de Biologie de l’ENS (IBENS), Département de biologie, École Normale Supérieure, CNRS, Inserm, Université PSL, Paris, France (S.L.).
14 Diabetology and Endocrinology Department, Bichat Hospital, Fédération de Diabétologie, France (L.P., A.C., R.R.).
15 Inserm, LNC UMR1231, Dijon, France (D.M.).
16 University of Bourgogne and Franche-Comté, LNC UMR1231, Dijon, France (D.M.).
17 FCS Bourgogne-Franche Comté, LipSTIC LabEx, Dijon, France (D.M.).
18 Plateau Automatisé de Biochimie, Dijon University Hospital, France (D.M.).
19 Dasman Diabetes Institute, Kuwait (F.A.).
# Contributed equally.