A research team from Paris Descartes University, Inserm and Sainte-Anne Hospital, led by Professor Marie-Odile Krebs, has demonstrated that epigenetic modifications accompany the onset of a psychotic episode in a cohort of young at-risk people aged 15–25 years. These modifications compromise systems for responding to oxidative stress and inflammation. Through this new work, the researchers have shed new light on this disease, for which the main biological explanation, before now, was based on disruption of dopamine secretion in the brain.
The study was published in Molecular Psychiatry on 26 April 2016
© fotolia
Psychotic disorders preferentially affect a young population, and have a major social impact. Several years before the onset of a true psychotic episode, certain changes in behaviour (isolation, aggressiveness), or certain non-specific (anxiety, problems with concentration or sleep) or more specific symptoms (perceptual abnormalities, fixed ideas, etc.) are generally present. Certain assessment tools have make it possible to define “at-risk mental state” criteria. Approximately one third of people with an “at-risk mental state” will develop a psychotic disorder within three years. There is therefore strong clinical relevance in understanding the physiopathological mechanisms that accompany this change, in order to better define monitoring strategies and, especially, therapeutic interventions.
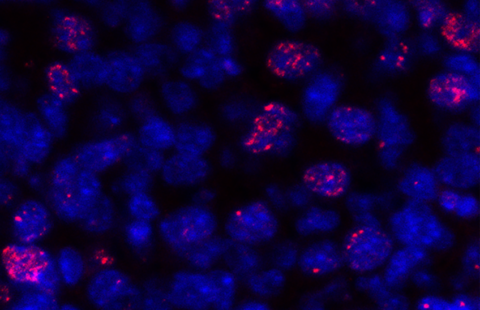
To study the onset of psychosis, the team of researchers adopted an original approach: they studied modifications in the methylation profile[1] (measured using a blood sample) of young at-risk subjects (ICAAR cohort), monitored for a period of one year. They compared the profiles of individuals who had experienced a psychotic episode with profiles of those who had not become ill. Their conclusions indicate that epigenetic modifications are involved in the onset of a psychotic episode. The modifications preferentially occurred in promoters of genes involved in protection against oxidative stress, in axonal guidance and in the inflammatory response.
Dynamic epigenetic changes accompany the onset of psychosis
The study was carried out on 39 young subjects, 14 of whom developed a psychotic transition in the year following their entry into the cohort. Analyses were concerned with over 400,000 methylation sites, distributed throughout the entire genome (also known as the “methylome”). They included the temporal dimension (comparison before and after the onset of psychosis), but also required the constitution of an appropriate control group (made up of young people who sought care and/or psychological support, but who did not meet the criteria of at-risk subjects). From the start of monitoring, people who went on to develop psychosis showed hypermethylation of the GSTM5 gene promoter[2]. During monitoring, hypomethylation of the GSTT1 gene promoter was observed, and hypermethylation of the GSTP1 gene. These three genes protect against oxidative stress. Other significant modifications were found in genes associated with inflammation and axonal guidance of neurons.
Approaches to developing molecular tools for early detection and targeted therapeutic agents
These results will lead to improved understanding of the biological upheavals that accompany the onset of psychosis. Until now, disruptions in dopamine secretion at brain level were the main physiopathological explanation for psychosis. With the help of these new data, its onset may be linked to an inflammatory or oxidative stress that disrupts the balance (homeostasis) that has already been weakened by a genetic, environmental or neurodevelopmental vulnerability. These results pave the way to the development of tests for the early detection of the illness and monitoring of its progress in these at-risk populations, since this disruption of homeostasis can be easily detected via blood samples, on a repeat basis if necessary. They also point to new therapeutic strategies aimed at preventing psychotic conversion.
[1] Epigenetic modifications are represented by biochemical tags present on the DNA. They do not modify the DNA sequence, but do, however, induce changes in gene activity. The best characterised are methyl groups (CH3: one carbon atom and three hydrogen atoms) attached to the DNA.
[2] A member of the glutathione transferase family, this gene encodes key enzymes that protect against oxidative stress.