The team led by Didier Leys and Régis Bordet (UMR-S 1171, Lille 2 University, Inserm, Lille University Hospital) has identified a biomarker that makes it possible to predict the risk of haemorrhagic complications from thrombolytic treatment following a Cerebrovascular Accident (CVA or stroke). This new marker could guide medical decision-making in difficult cases, particularly in severely affected patients, and thus help to prevent the risk of haemorrhage from thrombolysis.
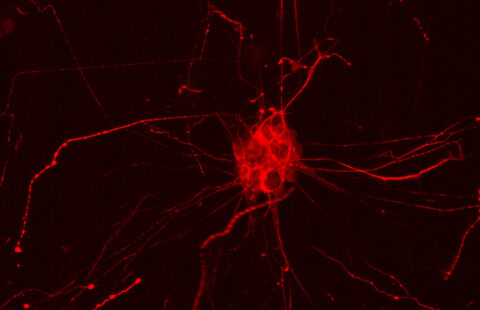
© Inserm, F. Koulikoff
During a stroke, thrombolysis is used to break up the clot obstructing an artery in the brain. For the last 15 years, this technique has been considered a major advance in the management of this condition. However, this treatment must be used within 4.5 hours of the onset of the stroke, if the benefit of relieving the blockage is not to be undone by the occurrence of intracerebral haemorrhage. This benefit/risk balance thus limits its use, because, according to current estimates, only 15% of patients are eligible for treatment. However, the clinical reality suggests that other patients might also benefit from thrombolysis, even if administered at a later time, without the risk of haemorrhage. Nonetheless, one still needs to be able to predict the risk of haemorrhagic complication, for a given patient, with the help of a marker.
The team led by Professors Leys and Bordet, which includes medical neurologists and pharmacologists, proposed that inflammation following stroke, and particularly interactions between the cells of the immune system and the vascular wall, might be responsible. They demonstrated the role of polymorphonuclear neutrophils, a type of cell involved in immune reactions, in the haemorrhagic effect of thrombolysis in the brains of animals, prior to testing the hypothesis in a cohort of 846 patients, comprising patients from Lille and from Finland.
The clinical results, which are published this week in the journal Neurology, show that a high concentration of polymorphonuclear neutrophils is associated with an increased risk of bleeding in the brain following thrombolysis, and a poorer prognosis at three months. By refining these results, the team of researchers in Lille revealed that the ratio of these neutrophils to another type of white blood cell, the lymphocytes, is even more predictive: a ratio greater than 4.8 is associated with a 4-fold higher risk.
This discovery should enable the launch of a clinical study to test the extension of the therapeutic window in patients with a ratio indicative of a lower risk, leading to personalised management guided by a simple biological marker, which can be measured routinely when the patient is admitted.
Understanding the mechanisms involved also offers an approach to preventing the risk of haemorrhage from thrombolysis by modulating the inflammatory cascade with drugs that are already on the market.
These contents could be interesting :