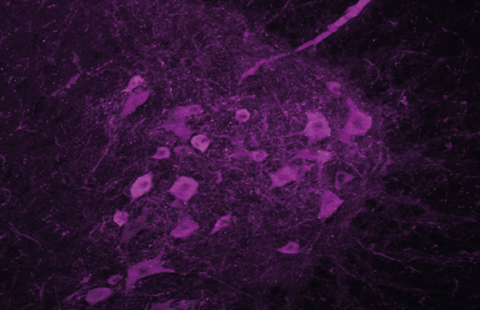
Visualisation, au sein de la barrière hémato-encéphalique, des macrophages associés au système nerveux central (CAM, en jaune), à l’interface entre un vaisseau sanguin (magenta) et des astrocytes (cyan), cellules de soutien des neurones en forme d’étoile. © Dr Damien Levard
Ageing greatly increases the risk of ischaemic stroke. A team of researchers from Inserm, Caen-Normandy University Hospital and Université de Caen Normandie have looked at the role that immune cells known as central nervous system-associated macrophages (CAMs) could play in the neurological damage that occurs following a stroke. Their research shows that during the course of ageing these cells acquire a key role in regulating the immune response triggered in the wake of a stroke. This research, to be published in Nature Neuroscience, highlights the importance of the presence of these cells at the interface between the blood and the brain in maintaining brain integrity.
The most common type of stroke is ischaemic stroke, which is caused by a blood clot obstructing an artery in the brain. Age is a major risk factor, with the risk of ischaemic stroke doubling every 10 years from the age of 55.
Ischaemic stroke is followed by inflammatory processes in the brain that may aggravate neurological lesions. Central nervous system-associated macrophages (CAMs) are immune cells located within the blood-brain barrier[1], at the interface between the blood circulation and the brain parenchyma[2]. Normally, the role of the CAMs is to monitor their environment, clean it of debris and other molecules from the brain parenchyma, as well as molecules from the blood that cross the blood-brain barrier, and alert other immune cells to the presence of pathogens. Little studied so far, they are nevertheless in an ideal anatomical situation to detect and react to external inflammatory signals and protect the brain parenchyma.
A research team from the Physiopathology and Imaging of Neurological Disorders unit (Inserm/Université de Caen Normandie) led by Marina Rubio, Inserm researcher, and Denis Vivien, professor and hospital practitioner at Université de Caen and Caen-Normandy University Hospital and head of the unit, has studied in mice and in human brain tissues how the role of CAMs evolves during ageing and their potential involvement in regulating the inflammatory response occurring in the brain after an ischaemic stroke.
First, the scientists sought to characterise how the role of CAMs and their biological environment change during the course of ageing. They observed that while the number of CAMs did not change with age, their functions did, with the appearance on their surface of the MHC II receptor – a specific molecule that plays a major role in the communication between immune cells (e.g. to coordinate the immune response to a pathogen). At the same time, the blood-brain barrier, which is intact in young brains, becomes more porous, allowing certain immune cells to pass from the blood to the parenchyma.
‘These observations suggest that the CAMs are capable of adapting their activity to the individual’s stage of life, state of health and the brain region in which they are located,’ specifies Rubio. Thus, in order to compensate for the age-related increase in blood-brain barrier porosity, they would strengthen their ability to communicate with other immune cells through further expression of the MHC II receptor. ‘Following an ischaemic stroke, this could help prevent an excessive immune response that would have more serious neurological consequences,’ adds the researcher.
The team then looked at the impact of these functional changes on the immune response in the brain parenchyma following an ischaemic stroke. To do this, it compared what happened after a stroke in a normal elderly mouse brain with what happened in the absence of CAMs or when their MHC II receptor was inhibited.
In these last two models, the researchers observed that during the acute phase of the ischaemic stroke and also in the days that followed, more immune cells from the blood crossed the blood-brain barrier, indicating its increased permeability coupled with an exacerbated immune response. This phenomenon was accompanied by a worsening of the neurological damage caused by the stroke.
‘These findings suggest that the CAMs acquire, during the course of ageing, a central role in orchestrating immune cell traffic after an ischaemic stroke, explains Vivien. And that, thanks to their capacity for adaptation, they ensure the ongoing close monitoring of the integrity of the blood-brain barrier and the intensity of the inflammatory response.’
The MHC II receptor located on the CAMs appears to be involved in this modulation as well as in the limitation of stroke-related neurological damage.
Further research for this team will aim to better understand the molecular mechanisms involved in the dialogue between the CAMs and the cells lining the internal wall of the brain’s blood vessels.
‘The objective will ultimately be to identify and develop new therapeutic targets that could enable the brain’s immune response to be modulated in a manner appropriate to each patient after a stroke,’ concludes Rubio.
[1]The blood-brain barrier separates the brain’s blood vessels from the brain parenchyma. It acts as a highly selective filter capable of allowing the passage of nutrients essential for the brain while protecting the parenchyma from pathogens, toxins and hormones circulating in the blood and which are likely to succeed in exiting the blood vessels.
[2]The parenchyma is the functional tissue of the brain directly involved in neural activities and the transmission of nerve impulses. It is surrounded by the perivascular spaces and the meninges where the CAMs reside.
These contents could be interesting :