Researcher Contact
Julien Marie
Inserm Research Director at the Cancer Research Center of Lyon
email: whyvra.znevr@vafrez.se
Telephone number provided upon request
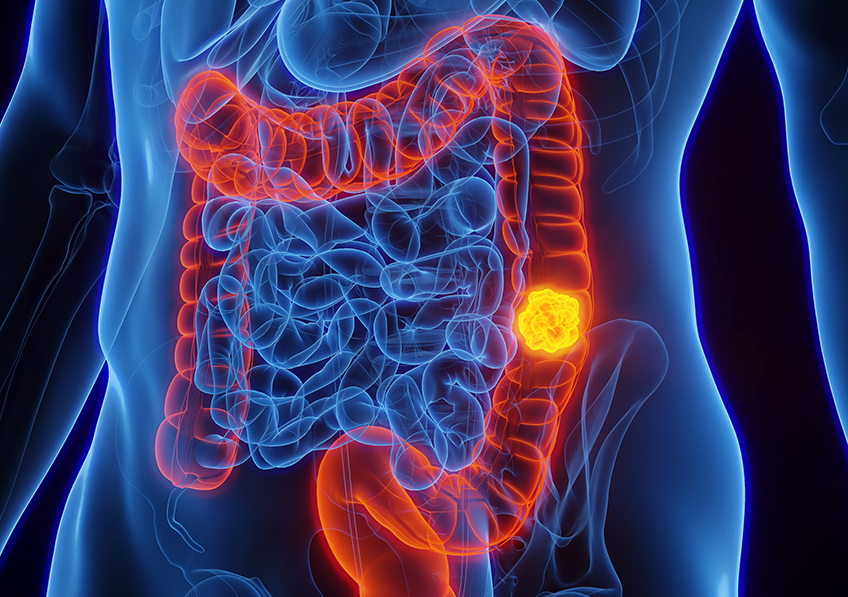 Around 30% of cancers develop in the wake of chronic localised inflammation. This is particularly the case of certain colorectal cancers, or cancers of the small intestine, liver or pancreas. © Adobe Stock
Around 30% of cancers develop in the wake of chronic localised inflammation. This is particularly the case of certain colorectal cancers, or cancers of the small intestine, liver or pancreas. © Adobe Stock
Nearly one in three cancers develops following chronic inflammation, whose origin remains unclear. In a new study, researchers from Inserm, CNRS, Université Claude-Bernard Lyon 1 and the Léon Bérard Centre at the Cancer Research Center of Lyon[1]identified lymphocytes involved in the inflammatory processes and that are thought to be implicated in the generation of these cancers. This research opens up new avenues in terms of prevention and treatment, and its findings have been published in Nature Immunology.
Around 30% of cancers develop in the wake of chronic localised inflammation. This is particularly the case of certain colorectal cancers, or cancers of the small intestine, liver or pancreas. However, many questions remained unanswered regarding their development. Is one specific immune cell responsible for the inflammatory process that leads to cancers, or more than one? And if so, which?
Answering these questions is one of the objectives of Inserm Research Director Julien Marie[2] and his team at the Cancer Research Center of Lyon (Inserm/CNRS/Université Claude-Bernard Lyon 1/Léon Bérard Centre) in order to better understand how the disease is initiated.
The researchers were particularly interested in TH17 lymphocytes – a population of immune cells which are already known to be involved in many inflammatory diseases, such as multiple sclerosis and Crohn’s disease.
Cells that cause cancer
The hypothesis was that TH17 cells are not a homogeneous population, but can actually be divided into several subgroups. Using single-cell RNA sequencing approaches, the scientists demonstrated this heterogeneity of TH17 cells within the gut.
‘More specifically, this study shows for the first time that there are actually eight TH17 subtypes with distinct roles. One of them has a tumorigenic role, which means that when certain activation barriers are removed, it will contribute to the development of cancers. On contact with these TH17 cells, the previously healthy gut cells become cancerous’, explains Marie.
The scientists then showed this tumorigenic population to be increased in patients at high risk of cancer. Finally, they also identified that a protein – cytokine TGF–β – is capable of inhibiting the formation of tumorigenic TH17 cells.
‘This study may make clinicians stop and think about the long-term use of immunotherapies in cancer patients, whose aim is to stimulate lymphocytes’, emphasises Marie.
While these therapies have transformed cancer care, they are also known to cause chronic gut inflammation. Therefore it is important to consider, for a given patient, the risks of immunotherapy being accompanied by the emergence of tumorigenic TH17 lymphocytes, which could eventually lead to the development of another cancer. Furthermore, this study lays the foundations for the development of new cancer preventive therapies by blocking the appearance of the TH17 subtype implicated by the scientists in this research.
[1]Scientists from the Institute of Molecular Genetics of Montpellier (CNRS/Université de Montpellier) also participated in this research.
[2]Julien Marie is the winner of the Bettencourt Coups d’Élan Prize for French Research.
Created by the Bettencourt-Schueller Foundation in 2000, this prize had been awarded to 78 French laboratories and over 900 researchers until 2021.
Julien Marie
Inserm Research Director at the Cancer Research Center of Lyon
email: whyvra.znevr@vafrez.se
Telephone number provided upon request
An intestinal TH17 cell-derived subset initiating cancer
Nature Immunology, August 2024
DOI : 10.1038/s41590-024-01909-7
Olivier Fesneau1*, Valentin Thevin1*, Valérie Pinet2, Chloe Goldsmith1 , Baptiste Vieille1, Saïdi M’Homa Soudja1, Rossano Lattanzio3, Michael Hahne2, Valérie Dardalhon2, Hector Hernandez Vargas1, Nicolas Benech1,4, and Julien C. Marie1,5$
1Cancer Research Center of Lyon INSERM U 1052, CNRS UMR 5286, Centre Léon Bérard, Claude Bernard Lyon1 University, Lyon, France
2 Institut de Génétique Moléculaire de Montpellier, Univ Montpellier, CNRS, Montpellier, France
3 Department of Innovative Technologies in Medicine & Dentistry, Center for Advanced Studies and Technology (CAST), G. d’Annunzio University of Chieti–Pescara, Chieti, Italy.
4 Hospices Civils de Lyon, Service d’hépato-gastroentérologie, Croix Rousse hospital, Lyon France
5 Equipe labellisée Ligue Nationale Contre le Cancer, Lyon France
*These 2 authors contributed equally to this work