Press Contact
Presse Institut Pasteur
Myriam Rebeyrotte 01 45 68 81 01
Marion Doucet 01 45 68 89 28
rf.ruetsap@esserp
Presse Inserm
Priscille Rivière 01 44 23 60 97
Juliette Hardy 01 44 23 60 98
Marine Leroy 01 44 23 60 73
rf.mresni@esserp
Erosive oral lichen planus (OLP) is an auto-immune disease affecting skin and mucous membranes which results in an abnormal immune response against mucocutaneous cells. Today, scientists at the Institut Pasteur, Inserm, Paul Sabatier University (Toulouse) and the CNRS have proven that the immune cells involved in OLP are the same as those activated during an immune response to human papillomavirus (type HPV-16). This suggests a link between OLP and HPV. The results of this study were published in the Journal of Investigative Dermatology.
Erosive oral lichen planus (OLP) is an inflammatory disease which is considered auto-immune because of the abnormal immune response it triggers against other cells in the body. The condition affects mucous membranes around the mouth and genitals causing lesions and the destruction of skin cells called keratinocytes. Because current treatments are only partially effective, the condition is chronic and, although rare (between 0.1 and 4% of the overall population is affected), OLP can have serious side effects such as pain, difficulty eating, and cancer.
Papillomavirus© Institut Pasteur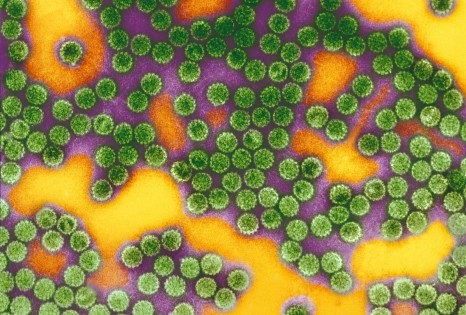
Little was known about the underlying biological mechanisms of OLP until teams led by Marie-Lise Gougeon (Institut Pasteur), Nicolas Fazilleau (Inserm, Paul Sabatier University, CNRS) and Hervé Bachelez (Sorbonne Paris Cité, Paris Diderot University) demonstrated that the immune response which leads to the destruction of mucosal cells involves the same lymphocytes responsible for the immune response to human papillomavirus (HPV). This would suggest a link between OLP and infection by the HPV-16 strain, a virus known to be responsible for genital warts and cervical cancer.
Initial analyses of lesional tissue and blood samples from OLP patients revealed the presence of cytotoxic lymphocytes around the destroyed cells. This prompted scientists to try to characterize the specific role and origin of these lymphocytes.
For the ten patients enrolled in a study by Manuelle Viguier (Institut Pasteur, Sorbonne Paris Cité, Paris Diderot University), analyses showed an abnormally high population of a particular type of lymphocyte specific for HPV-16: T CD8 (type Vβ3).
The proportion of this type of lymphocyte was then measured during the different phases of OLP (outbreaks or remission stages). This allowed the scientists to show that the number of these cells decreased during periods of clinical remission and multiplied during outbreaks.
One of the theories put forward by the scientists was that keratinocytes in OLP patients might express an autoantigen (an endogenous normal tissue constituent) very similar to the HPV-16 antigen. This could be a source of confusion for T lymphocytes which, having already been exposed to HPV, might mistake the surface antigen on keratinocytes of OLP patients for the HPV antigen and trigger a cytotoxic immune response against keratinocytes.
This research indicates that the auto-immune disease OLP could involve T CD8 lymphocytes specific to HPV-16. This is the first time a link has been established between infection by HPV-16 and an auto-immune disease.
These results open up new therapeutic possibilities for treating severe forms of OLP. The Institut Pasteur has filed to patent this research in hopes that use of the HPV vaccine will be expanded to include OLP.
This study was financed by the French Dermatological Society, the Fondation ARC (Cancer Research Foundation), the French Cancer League, the French National Cancer Institute, the Midi-Pyrénées Regional Council and the Marie Curie International Re-integration Grant.
Presse Institut Pasteur
Myriam Rebeyrotte 01 45 68 81 01
Marion Doucet 01 45 68 89 28
rf.ruetsap@esserp
Presse Inserm
Priscille Rivière 01 44 23 60 97
Juliette Hardy 01 44 23 60 98
Marine Leroy 01 44 23 60 73
rf.mresni@esserp
Peripheral and Local Human Papillomavirus 16-specific CD8+ T-cell expansions characterize erosive oral lichen planus, Journal of Investigative Dermatology, 10 septembre 2014, http://www.nature.com/jid/journal/vaop/naam/pdf/jid2014397a.pdf
Manuelle Viguier(1,2*), Hervé Bachelez(2,3*), Béatrice Poirier(1), Jérémy Kagan(4,5,6,7), Maxime Battistella(1,8), François Aubin(9), Antoine Touzé(10), Maryvonnick Carmagnat(11), Camille Francès(12), Marie-Lise Gougeon(1+) and Nicolas Fazilleau(4,5,6,7+).
(1) Institut Pasteur, Antiviral Immunity Biotherapy and Vaccine Unit, Paris, France.
(2) Sorbonne Paris Cité Université Paris Diderot, Paris, France.
(3) Université Paris Descartes, Imagine Institute, Necker Hospital, Paris, France.
(4) Centre de Physiopathologie de Toulouse Purpan, Toulouse, F-31300, France.
(5) INSERM, U1043, Toulouse, F-31300, France.
(6) CNRS, UMR5282, Toulouse, F-31300, France.
(7) Université Toulouse III Paul-Sabatier, Toulouse, F-31300, France.
(8) INSERM, UMR-S728, Université Paris Diderot, Paris, F-75010, France.
(9) Université de Franche Comté, EA3181, SFR FED 4234, Centre Hospitalier Universitaire, Service de Dermatologie, Besançon, France.
(10) UMR 1282 INRA-Université François Rabelais, Tours, France.
(11) Laboratoire d’Immunologie, Hôpital Saint-Louis, Paris, France.
(12) Service de Dermatologie-Allergologie, APHP, Hôpital Tenon, Université Paris VI, 4 rue de la Chine, 75020 Paris, France.
* Ces auteurs ont contribué équitablement à ce travail.
+ Ces auteurs ont contribué équitablement à ce travail.