Researcher Contact
Jennifer Zeitlin
Epidemiologist and research director at Inserm
U 1153 – Centre de recherche épidémiologie et statistiques (CRESS)
 France’s most deprived municipalities have the highest newborn death rates according to the study’s social deprivation index adjusted for the perinatal period (illustration) © Adobestock
France’s most deprived municipalities have the highest newborn death rates according to the study’s social deprivation index adjusted for the perinatal period (illustration) © Adobestock
With neonatal mortality on the increase in France, a new study by Inserm, Paris Cité University, Inrae, Paris Nord University and APHP, published on 16 September in BMJ Medicine, shows that it could be linked to socioeconomic inequalities. Using their social deprivation index adjusted for the perinatal period, the researchers observed that the risk of neonatal death is higher for mothers living in deprived municipalities. These findings emphasise the importance of conducting perinatal care audits across France, according to the researchers.
Women living in socioeconomically disadvantaged municipalities are more likely to see their child die in the first few days after birth. This is the finding of a new study published by a research team from Inserm, Paris Cité University, Inrae, Paris Nord University and APHP in BMJ Medicine on 16 September 2025.
A study from 2022[1] had already revealed a significant increase in infant mortality (death before one year of age) in France since 2012. While this study had identified neonatal mortality (death within the first 28 days of life) as the main component in the increase in infant mortality, it did not make it possible to know the areas and populations most affected.
To remedy this, a scientific team has developed a social deprivation index adjusted for the perinatal period for each municipality in mainland France[2], resulting from the analysis of various factors associated with the health of newborns in previous studies: unemployment rate, percentage of immigrants in the sector, that of tenants, single-parent families, and median household income. The scientists then cross-referenced this indicator with the neonatal mortality rate over two periods: 2001-2008 and 2015-2020, using the French National Health Data System (SNDS).
The results highlight significant inequalities in neonatal mortality.
“Regardless of the period studied, our social deprivation index adjusted for the perinatal period shows more deaths occurring in newborns whose mothers live in the most deprived municipalities,” observes Jennifer Zeitlin, epidemiologist and research director at Inserm, and last author of the study.
When analysing the data in more detail, the scientists saw that over the 2015-2020 period, the 20% of children born to mothers living in the most deprived municipalities (according to the social deprivation index adjusted for the perinatal period) had a death rate in the 28 days following birth of 3.34 per 1 000 live births, i.e. a risk around 1.7 times that of the 20% of children from the most least deprived areas (1.95 deaths per 1 000 births). The more mothers come from deprived areas, the greater the risk of neonatal death.
“If the entire population had the same risk of neonatal mortality as the 20% least deprived, it is estimated that around a quarter of deaths, i.e. 2 496 newborn deaths, could have been avoided in the 2015-2020 period alone”, says Victor Sartorius, the first author.
The comparison between the periods 2001-2008 and 2015-2020 confirms the increase in neonatal mortality in mainland France. But “the increase observed is concentrated only in deprived areas, while mortality has remained stable in the rest of the country”, observes Zeitlin.
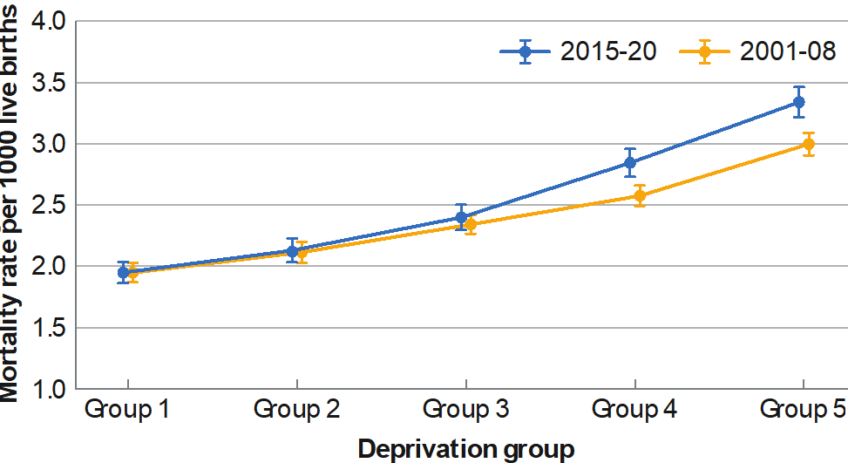
Title: Neonatal mortality rates in mainland France between 2015 and 2020 and 2001 and 2008 according to social deprivation groups
Caption: To analyse the link between neonatal mortality and social deprivation, the statisticians divided births into five equal groups called “quintiles”, according to the social deprivation index adjusted for the mothers’ perinatal period, over two periods: between 2001 and 2008, and between 2015 and 2020. The first quintile (group 1) corresponds to the 20% of children born to mothers living in the least deprived municipalities, and the last quintile (group 5) to the 20% of children born to mothers living in the most deprived municipalities. When comparing the 2001-2008 period with that of 2015-2020, the researchers observed that the neonatal mortality rate remained stable in the least deprived groups (1 and 2) and the median group (3). However, they observed an increase in the mortality rate between these two periods, which is concentrated exclusively in the most deprived groups (4 and 5). This distribution highlights inequalities in relation to neonatal mortality according to the social deprivation of the mothers.
Several hypotheses can be put forward to explain the association between the level of social deprivation and neonatal mortality. For example, characteristics that have been linked to socioeconomic level, such as overweight, smoking and exposure to pollution, lead to a higher risk of prematurity or low birth weight in the baby, which are themselves risk factors for neonatal death. There are also ethical and personal considerations such as the decision whether or not to terminate the pregnancy due to certain foetal diseases.
“We also need to mention the organisation of our healthcare system; we know that access to healthcare and the ability of residents to use the healthcare system is reduced in deprived areas, adds Sartorius. In addition, high occupancy rates in units that care for critically ill newborns together with under-staffing could also be a hypothesis among the causes to be explored.”
“According to a recent analysis by the French National Authority for Health (HAS), 57% of serious adverse events related to care in newborns, such as deaths, could have been avoided[3], reiterates Zeitlin. The question is therefore how to improve the organisation of healthcare provision and the conditions for patient care, particularly in the most fragile areas according to our social and perinatal deprivation index. This could include more staff, better training of healthcare workers and appropriate infrastructure.”
To mitigate the risks, the research team suggests conducting audits of perinatal care provision in each area, like the one whose conclusions were made public in 2015 in Seine-Saint-Denis[4].
“Our study shows the extent to which deprived populations are at the forefront of neonatal mortality and highlights the urgency of implementing targeted public health measures in the high-risk areas that we’ve identified”, concludes the last author.
[1]https://doi.org/10.1016/j.lanepe.2022.100339
[2]Except for municipalities with fewer than 50 households, for which the data were not available.
[3]evenements_indesirables_graves_associes_aux_soins_eigs_survenus_chez_les_nouveau-nes.pdf
[4]Fresh insight into the causes of infant and perinatal mortality in the Seine-Saint-Denis district – Inserm press room
Jennifer Zeitlin
Epidemiologist and research director at Inserm
U 1153 – Centre de recherche épidémiologie et statistiques (CRESS)
Area-based socioeconomic inequalities contribute to rising neonatal mortality rates: a study of national routine birth data in France
Victor Sartorius, MD1,2; Héloïse Torchin, MD, PhD1,3; Luc Gaulard, MSc1; Marianne Philibert, MSc1; Victoria Butler, MD1,3; Monica Saucedo, MD, PhD1; Catherine Deneux-Tharaux, MD, PhD1; Jeanne Fresson, MD1,4; Jennifer Zeitlin, PhD1.
BMJ Medicine, 15 September 2025