Fotolia
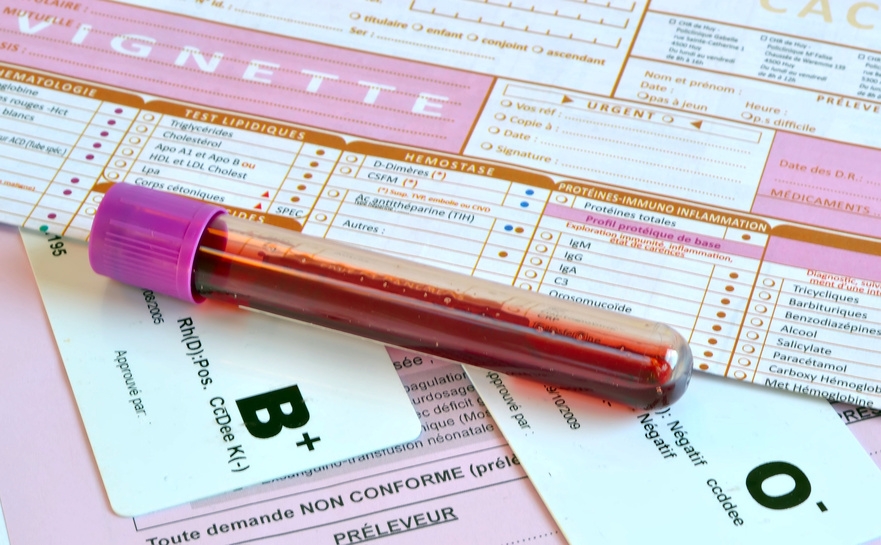
Teams from the AP-HP Paris public hospitals network, in collaboration with researchers from the Brain & Spine Institute (ICM) (Inserm/CNRS/UPMC), and Metafora biosystems, a start-up with links to the CNRS, have recently developed a diagnostic blood test for a rare but treatable condition called De Vivo disease.
It was tested on 30 patients with the disease, which causes neurological deficits such as epilepsy and movement disorders.
Compared with current diagnostic tests that use an invasive procedure (lumbar puncture) or complex DNA analysis, this new test[1], the results of which have been published in Annals of Neurology, will be able to screen for the condition rapidly (within 48h) and with ease in both adults and children.
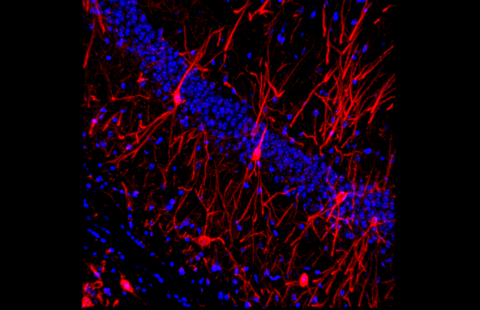
De Vivo disease or glucose transporter type 1 deficiency syndrome (GLUT1-DS) is most often characterized by developmental delay, epilepsy and/or movement disorders in children. Formes frustres[2] have been described in children (abnormal movement episodes) but also in adults. On the basis of an estimated prevalence of 1/83,000 in the Danish population, the number of those affected in the French population[3] is thought to be 800, a little over one hundred of whom will be diagnosed. Once diagnosed, metabolic therapies are available to alleviate the symptoms.
Dr Fanny Mochel from AP-HP Pitié-Salpêtrière University Hospital, along with teams from other hospitals of the AP-HP network (Bichat, Raymond-Poincaré and Robert-Debré) and the Brain & Spine Institute (Inserm/CNRS/UPMC), have developed a simple and rapid (within 48h) diagnostic blood test for De Vivo in collaboration with Metafora biosystems. Current diagnosis is restrictive because it involves an invasive procedure (lumbar puncture) and complex genetic analysis.
In this study, blood samples from 30 De Vivo patients, with profiles differing according to age and symptoms, were analyzed. Following comparison with samples from 346 healthy controls, the results show that the test is significantly conclusive in that it identified 78% of the De Vivo patients, including those for whom the genetic analysis was inconclusive.
Backed by these results, the researchers recommend the use of this new test in routine clinical practice in all neuropediatric and neurology departments. They suggest that its simplicity should enable more patients to be diagnosed in France.
Thanks to this innovative novel blood test, it will be possible to screen for the disease in all patients presenting with cognitive impairment, movement disorders, epilepsy or a combination of the three. The therapies at our disposal can considerably improve symptoms, including, for example, the control of epileptic seizures. However, since these are more effective when started early, timely diagnosis of the condition is crucial.
[1] Protected by patent CNRS WO2004/096841.
[2] When patients do not present all the characteristic symptoms of a disease or when such symptoms are mild
[3] [1] Larsen J, et al. The role of SLC2A1 mutations in myoclonic astatic epilepsy and absence epilepsy, and the estimated frequency of GLUT1 deficiency syndrome. Epilepsia. 2015 Dec;56(12):e203-8.