A small number of patients infected by HIV spontaneously control viral replication without antiretroviral therapy, and do not develop the disease. The ability of these rare patients, known as “HIV controllers”, to suppress HIV replication appears to be down to a highly effective immune response. Scientists from the Institut Pasteur and Inserm observed that CD4+ T immune cells in these patients, recruited from the ANRS CO21 CODEX cohort, were capable of recognizing tiny quantities of the virus. This highly sensitive detection is dependent on the expression of specific T cell receptors on the surface of immune cells, which target the HIV capsid protein with high affinity. The preferential expression of these receptors appears to keep the immune system on a constant state of alert, thereby enabling the patients to control HIV. These findings have been published in The Journal of Clinical Investigation.
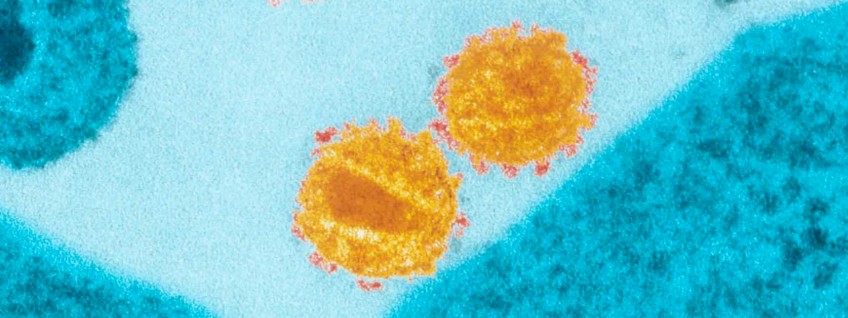
© Institut Pasteur, Charles Dauguet
“HIV controller” patients represent less than 0.5% of all HIV-infected patients. They are proof that in some cases the human immune system can resist the harmful effects of HIV. They are able to maintain a population of functional auxiliary CD4+ T lymphocytes, whereas in patients that have gone on to develop the disease these cells are destroyed or rendered inactive. The patients enrolled in the HIV controller study were recruited from the ANRS CO21 CODEX cohort which includes the few HIV controller patients living in France. Scientists in the team led by Lisa Chakrabarti (Viral Pathogenesis Unit at the Institut Pasteur / Inserm unit U1108), in collaboration with Olivier Lambotte from Bicêtre Hospital, used the cohort to analyze the CD4+ T cell responses of these patients at molecular level.
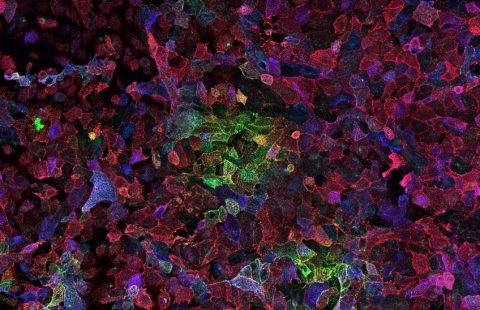
To trigger the antiviral immune response, the CD4+ T cells of HIV controllers are able to produce numerous cytokines in response to very low doses of HIV antigens. The study revealed that these highly sensitive responses were due to the expression of particular T cell receptors (TCRs) on the surface of the controllers’ CD4+ T cells. In comparison, these TCRs were rarely found on the CD4+ T cells of patients receiving treatment. The scientists showed in particular that the TCRs targeting Gag293, the HIV capsid’s most highly conserved peptide, frequently shared the same sequence in HIV controllers. These “public” TCRs have a strong affinity for the Gag293 peptide, when this peptide is presented at the surface of immune cells. This strong affinity interaction ensures the highly sensitive detection of infected cells in HIV controllers. Transferring these TCRs to healthy cells reproduces the properties typically associated with CD4+ T cells in HIV controllers, with highly sensitive responses and the production of multiple cytokines.
Overall, this research shows that the expression of high-affinity TCRs is linked with spontaneous control of HIV infection. Immunotherapy strategies based on transferring or boosting these TCRs could help restore effective antiviral responses in patients that have gone on to develop the disease.
This research was funded by the ANRS (France REcherche Nord & Sud Sida-HIV Hépatites), the French National Research Agency (ANR), the Institut Pasteur, the Australian Research Council (ARC) and the Australian National Health and Medical Research Council (NHMRC).
These contents could be interesting :
- Institut Pasteur, Viral Pathogenesis Unit, Paris, France.
- INSERM U1184, Center for Immunology of Viral Infections and Autoimmune Diseases, Paris, France.
- Assistance Publique – Hôpitaux de Paris (AP-HP), Department of Internal Medicine and Clinical Immunology, University Hospital Paris Sud, Le Kremlin-Bicêtre, France.
- Université Paris Sud, UMR1184, Le Kremlin-Bicêtre, France.
- CEA, DSV/iMETI, Division of Immuno-Virology, IDMIT, France.
- Infection and Immunity Program and Department of Biochemistry and Molecular Biology, Biomedicine Discovery Institute, and
- Australian Research Council Centre of Excellence for Advanced Molecular Imaging, Monash University, Clayton, Victoria, Australia.
- Institut Pasteur, Department of Immunology, Paris, France.
- INSERM U1018, Center for Research in Epidemiology and Population Health (CESP), Le Kremlin-Bicêtre, France.
- Institut Pasteur, Genomic Bioanalysis Group, Paris, France.
- Raymond Poincaré Hospital, AP-HP, Infectious and Tropical Diseases Department, Garches, France.
- Institute of Infection and Immunity, School of Medicine, Cardiff University, Cardiff, Wales, United Kingdom.
- INSERM U1108, Paris, France.