Benzodiazepines are prescribed to treat symptoms of anxiety and sleeping disorders. Collaborative research conducted by researchers from three Inserm units in Bordeaux has recently highlighted the link between benzodiazepine use and the development of dementia in the over 65s. The researchers analysed a sample from the PAQUID[1] cohort, consisting of individuals with a mean age of over 78, who were monitored for 15 years. The results from comparative analysis of this population demonstrate the risk of developing dementia increased by 50% for subjects who consumed benzodiazepines during the follow-up period, compared with those who had never used benzodiazepines. Although this study does not confirm a cause and effect relationship, as is the case for all epidemiological research, the researchers recommend increased vigilance when using these molecules, which remain useful in the treatment of insomnia and anxiety in elderly patients.
In France, approximately 30% of individuals over 65 are prescribed benzodiazepines to treat the symptoms of anxiety and sleep disorders. The prescription of these molecules is widespread, especially in France and other countries such as Canada, Spain and Australia. Consumption of benzodiazepines is often chronic, with many people taking them over a period (often several years) that significantly exceeds recommended good practice guidelines that suggest limiting the duration to two to four weeks. The effects of benzodiazepines on cognition have been the subject of several studies with much-debated results.
On 28 September 2012, researchers from Inserm unit 657 “Pharmacoepidemiology and the assessment of the impact of health products on the population”, 897 “Inserm Research Centre into epidemiology and biostatistics” and 708 “Neuroepidemiology”, in collaboration with the Université de Bordeaux, published on-line the sophisticated results of analyses from a cohort of elderly individuals to improve knowledge of the relationship between the use of benzodiazepines and the development of dementia.
In an attempt to counteract the bias that may have restricted the scope of previous studies, the researchers completed several comparative analyses using data from the PAQUID cohort, covering 3777 individuals from between 1897 and 1989.
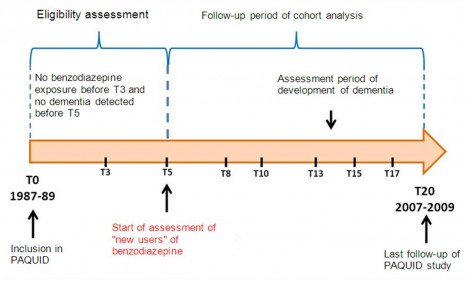
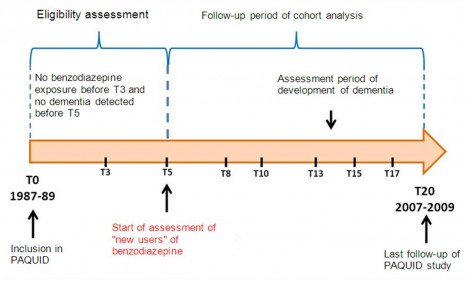
Diagram: Study design for cohort analyses
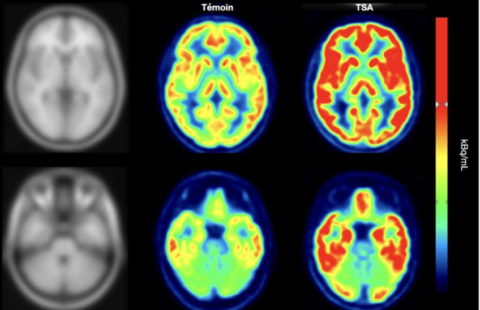
© Inserm / J.Hardy
The main study focused on a sample of 1063 individuals from the PAQUID cohort (mean age of 78), who were free from dementia symptoms at the beginning of the follow-up period and who had not consumed any benzodiazepines prior to the fifth year in the follow-up period (see above diagram). Out of the 1063 individuals, 95 used benzodiazepines from the fifth year onwards, thus defining two populations: those “exposed to benzodiazepines” and those “not exposed to benzodiazepines”. The annual occurrence of dementia observed in the exposed group is 4.8 individuals out of 100, compared with 3.2 individuals out of 100 for the “non-exposed” group.
“The analysis of the cases of dementia in the first population group shows that individuals who began treatment after five years during the follow-up period had an increased risk of developing dementia” states Tobias Kurth, an Inserm research director. “We wanted to check the robustness of this result by completing two additional analyses” he adds.
The second analysis consisted of creating five “small” cohorts using the sample studied previously. The researchers demonstrated that the link between benzodiazepine and dementia is robust, although the date treatment began does vary (benzodiazepine consumed from T5, T8, T10, T13, and T15).
To supplement these results, the researchers completed a case-control study on 1633 individuals with dementia (case) and 1810 without any dementia symptoms (control), all taken from the initial PAQUID population. For each time T studied, each case was compared with one or several individuals from the control group. This last analysis confirmed the trend observed in the main study, regardless of the previous exposure duration (three to five years for recent users to more than 10 years for users who had always taken benzodiazepines during the follow-up period).
“According to our analysis, benzodiazepine exposure for the over-65s is linked to an increased risk of dementia. Although we cannot prove a cause and effect relationship, we observed that during the follow-up period benzodiazepine users had a risk of developing dementia that was 50% higher than those who had never taken benzodiazepine”
indicates Bernard Bégaud.
Although these molecules are useful to treat insomnia and anxiety, the authors of this study indicate that their consumption may lead to adverse effects, such as falls. Since this new data confirms that from the four previous studies, the researchers recommend “limiting prescriptions to periods of a few weeks and taking care to ensure these molecules are used correctly. We doubt that consumption over a period of a few weeks can have a negative impact on the risk of dementia”, concludes Bernard Bégaud. Furthermore, additional studies would also make it possible to ascertain whether this link is found in persons aged under 65.
[1] PAQUID (Personnes Agées QUID), cohort launched in 1988, of a population of subjects living in their own homes in two départements in South-West France, la Gironde and la Dordogne.
3777 subjects aged 65 and over took part in the study.
These contents could be interesting :