 © Adobe stock
© Adobe stock
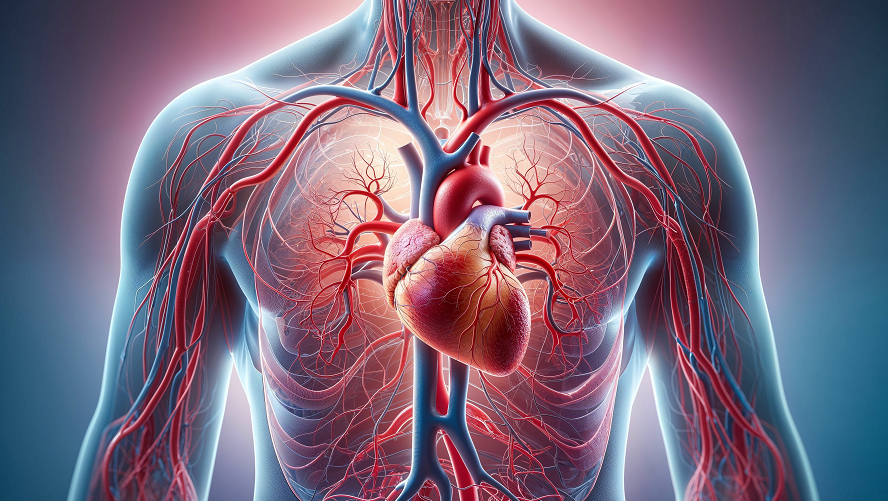
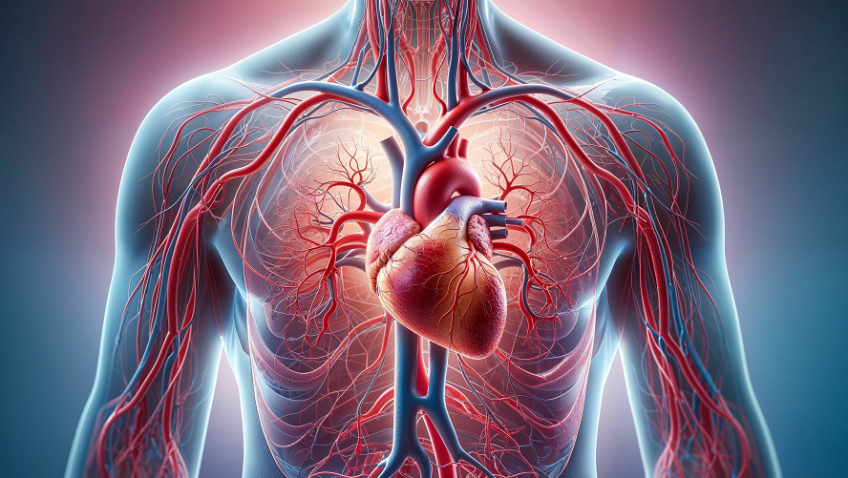
Cardiovascular diseases represent the leading cause of death worldwide[1]. Preventing cardiovascular risk by identifying the people most susceptible to these diseases is a major public health challenge. In a new study in this field, researchers from Inserm, Université de Lorraine and Nancy Regional University Hospital opted to focus on arterial stiffness and how it changes with age, given that ageing is associated with a loss of arterial flexibility. Thanks to health data collected from over 1,250 Europeans, their research confirms that the stiffer the arteries, the greater the cardiovascular risk. The scientists suggest measuring arterial stiffness as a way to predict a patient’s cardiovascular risk, and emphasise the utility of a specific clinical tool called the Cardio-Ankle Vascular Index (CAVI). These findings have been published in eBioMedicine.
Cardiovascular risk is the probability of developing a cardiovascular disease or accident (problems affecting the heart and arteries). Finding a measurement that can predict this risk through the early detection of the factors that can influence it is a major challenge for research. The risk factors that are already well-known are high blood pressure, smoking, diabetes, high cholesterol, excess weight and sedentary lifestyle.
Previous studies have shown that ageing affects the flexibility of our arteries in that they become increasingly rigid over time. What is more, the scientific literature indicates that this phenomenon may be accelerated by other factors during ageing, such as hypertension or diabetes, and is associated with an increased cardiovascular risk. On the basis of these factors, it had been suggested that looking at arterial stiffness could be useful in preventing cardiovascular risk. However, testing for arterial stiffness is not on the list of recommended clinical practices.
In a new study, researchers from Inserm, Université de Lorraine and Nancy Regional University Hospital looked at a tool for measuring arterial stiffness called the Cardio-Ankle Vascular Index (CAVI), hypothesising that its use in clinical practice could predict patient cardiovascular risk.
The scientists were specifically interested in CAVI because of its accuracy, non-invasiveness and the fact that it is not influenced by blood pressure but reflects the structure of the artery itself. CAVI is measured using four cuffs – one around each arm and one around each ankle – assessing stiffness from the femoral artery to the tibial artery. A microphone is also placed on the heart. The tool measures the speed of blood flow and calculates an index: the higher the number, the stiffer the arteries[2].
During their research, the scientists followed 1,250 people from 18 European countries, all over the age of 40[3]. They provided their medical history and underwent a physical examination, including an assessment of their arterial stiffness using CAVI. They were then invited for a follow-up examination 2 years after the first measurement, and for some, up to 5 years after the first measurement. The aim of the follow-up was to assess the progression of the arterial stiffness and correlate this with the participants’ general state of health.
Thanks to their measurements, the researchers were able to observe that each one-point increase in CAVI, which corresponds to an approximate 10% increase in arterial stiffness, was associated with a 25% increased risk of a cardiovascular event in the years following the measurement.
The researchers also looked at what might influence arterial stiffness. They saw that age affected not just the CAVI value but also its progression, in that it increases more rapidly with age. They also observed the impact of blood pressure: the higher the blood pressure, the higher the CAVI.
The scientists then tried to determine a threshold for arterial stiffness that would be associated with an increased cardiovascular risk and could be commonly recognised and adopted by clinicians, in order to implement more intensive patient monitoring. They found that a CAVI of over 9.25 was associated with a high cardiovascular risk from the age of 60.
Finally, they observed that treatment for cholesterol or diabetes affected the rate of progression of arterial stiffness. Although these observations are still being studied, they do suggest that certain treatments could help slow the progression of arterial stiffness.
‘Our findings suggest that CAVI could be a quick, easy and non-invasive tool for predicting cardiovascular risk. In the future, it could be included on the list of tests recommended in clinics to predict a person’s cardiovascular risk and provide preventive monitoring,’ explains Magnus Bäck, first author of the study.
‘As well as being easy to deploy, we could use CAVI to determine the actual age of the cardiovascular system,’ explains Athanase Benetos, the study’s final author.
[1] WHO data: https://www.who.int/fr/health-topics/cardiovascular-diseases#tab=tab_1
[2] An index of 10 is already a sign of great rigidity.
[3] TRIPLE-A-Stiffness is an international longitudinal cohort study having recruited more than 2,000 participants over 40 years of age from 18 European countries. Of these, 1,250 subjects (55% of whom women) were followed for a median duration of 3.82 (2.81 – 4.69) years.