©fotolia
Researchers from Généthon, the AFM-Téléthon laboratory, Inserm (UMR 1089, Nantes) and the University of London (Royal Holloway) demonstrated the efficacy of an innovative gene therapy in the treatment of Duchenne muscular dystrophy. Indeed, after injecting microdystrophin (a “shortened” version of the dystrophin gene) via a drug vector, the researchers managed to restore muscle strength and stabilise the clinical symptoms in dogs naturally affected by Duchenne muscular dystrophy. A first. This work, published today in Nature Communications, has been achieved thanks to donations from the French Téléthon.
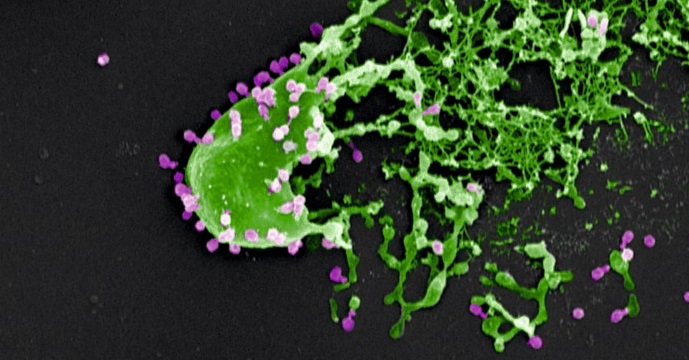
Duchenne muscular dystrophy is a rare progressive genetic disorder involving all the muscles of the body, and affects 1 in 5,000 boys. It is the most common neuromuscular disorder in children. It is associated with abnormalities in the DMD gene, which encodes dystrophin, a protein that is essential for proper muscle function. This gene is one of the largest in our genome (2.3 million base pairs, of which over 11,000 are coding). Because of this size, it is technically impossible to insert the entire DNA for dystrophin into a viral vector (or even the 11,000 coding base pairs alone), as is usually done for gene therapy.
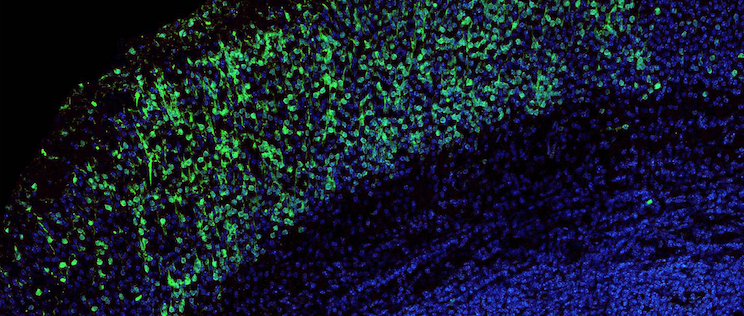
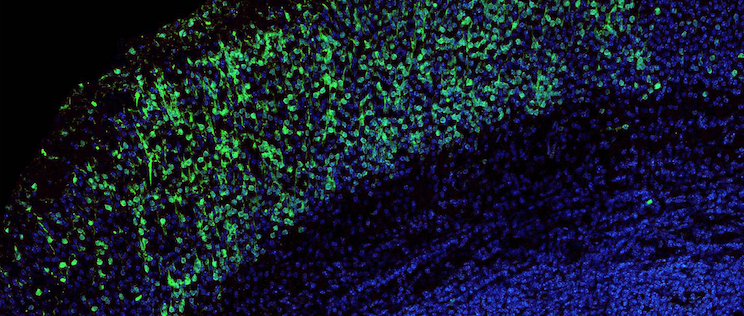
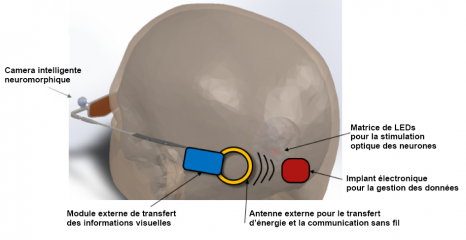
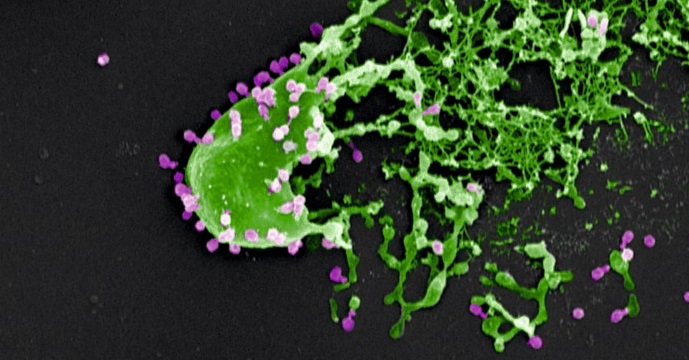
To meet this challenge, teams at Genethon developed, in collaboration with a team at Royal Holloway University of London led by Pr. Dickson, and produced, a gene therapy drug combining an AAV-type viral vector with a shortened version of the dystrophin gene (approximately 4,000 base pairs), allowing the production of a functional protein. Dr Le Guiner’s team tested this innovative treatment in 12 dogs naturally affected by Duchenne muscular dystrophy.
By injecting this microdystrophin intravenously, and hence into the whole body of the dogs, the researchers observed that dystrophin expression returned to a high level, and muscle function was significantly restored, with stabilisation of the clinical symptoms observed for over 2 years following injection of the drug (see video). No immunosuppressive treatment was administered beforehand, and no side-effects were observed.
Some Golden Retrievers develop Duchenne muscular dystrophy naturally. The successful treatment of these dogs, which show the same clinical symptoms as children with this disease, and are of a similar weight, is a decisive step toward developing the same treatment in children.
“This preclinical study demonstrates the safety and efficacy of microdystrophin, and makes it possible to consider developing a clinical trial in patients. Indeed, this is the first time that it has been possible to treat the whole body of a large-sized animal with this protein. Moreover, this innovative approach allows treatment of all patients with Duchenne muscular dystrophy, regardless of the genetic mutation responsible,” says Caroline Le Guiner, the main author of this study.
“This is tremendously exciting progress towards a gene therapy for DMD. The studies in GRMD dogs have been spectacular and exceeded our expectations. My team has worked for many years to optimise a gene therapy medicine for DMD, and now the quite outstanding work of colleagues in France, in Genethon, in Nantes and in Paris has taken us close to clinical trials in DMD patients. I pay thanks also to the amazing and steadfast support of this research by AFM-Telethon and MDUK (Muscular Dystrophy UK) which has been essential to this achievement.” commented George Dickson.
For Frédéric Revah, Chief Executive Officer of Généthon: “For the first time, researchers obtained a systemic therapeutic effect on a neuromuscular disease in dogs using microdystrophin, and without immunosuppressive treatment. This highly complex cutting edge technology has been developed as part of an exceptional collaborative effort between Genethon and academic teams from Britain and France. Now our bioproduction experts have the task of producing a sufficient quantity of these new drug vectors, under GMP conditions, for the clinical trial.”
“This new evidence of the efficacy of gene therapy in Duchenne muscular dystrophy strengthens the therapeutic arsenal developed (exon skipping, CRISPR Cas-9, pharmacogenetics, etc.), and the first results are there. We need to forge ahead to complete the final phase and transform these scientific advances into drugs for children,” emphasises Serge Braun, Scientific Director of AFM-Téléthon.