Research jointly conducted by investigators at Institut Gustave Roussy, Inserm, Institut Pasteur and INRA (French National Agronomic Research Institute) has led to a rather surprising discovery on the manner in which cancer chemotherapy treatments act more effectively with the help of the intestinal flora (also known as the intestinal microbiota). Indeed, the researchers have just shown that the efficacy of one of the molecules most often used in chemotherapy relies to an extent on its capacity to mobilise certain bacteria from the intestinal flora toward the bloodstream and lymph nodes. Once inside the lymph nodes, these bacteria stimulate fresh immune defences which then enhance the body’s ability to fight the malignant tumour.
Results of this work are published in the journal Science on 22 November 2013.
©Fotolia
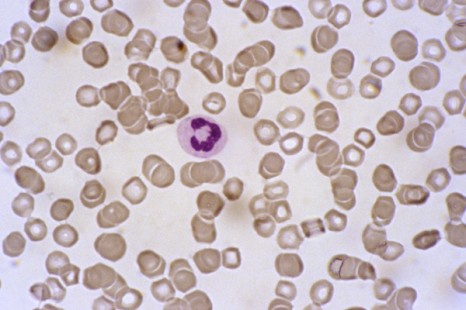
The intestinal microbiota is made up of 100,000 billion bacteria. It is a genuine organ, since the bacterial species that comprise it carry out functions crucial to our health, such as the elimination of substances that are foreign to the body (and potentially toxic), or keeping the pathogens that contaminate us at bay. They also ensure the degradation of ingested food, for better intestinal absorption and optimal metabolism. These millions of bacteria colonise the intestine from birth, and play a key role in the maturation of the immune defences.
However, the bacterial species that make up the intestinal microbiota vary from one individual to another, and the presence or absence of one or another bacterial species seems to influence the occurrence of some diseases, or, conversely, may protect us.
In the cancer area, the French team directed by Prof Laurence Zitvogel, Director of Inserm Unit 1015, “Tumour Immunology and Immunotherapy,” at Institut Gustave Roussy, in close collaboration with Institut Pasteur (Dr Ivo Gomperts Boneca, “Biology and Genetics of the Bacterial Cell Wall” Unit) and researchers at INRA (Drs Patricia Lepage and Joël Doré, Micalis Unit, “Food Microbiology in the Service of Health”), has just provided evidence that the intestinal flora stimulates an individual’s immune responses to combat cancer during chemotherapy.
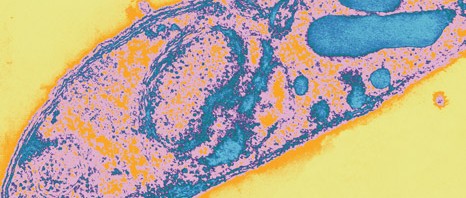
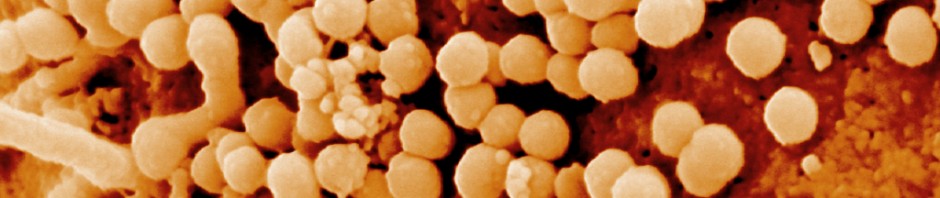
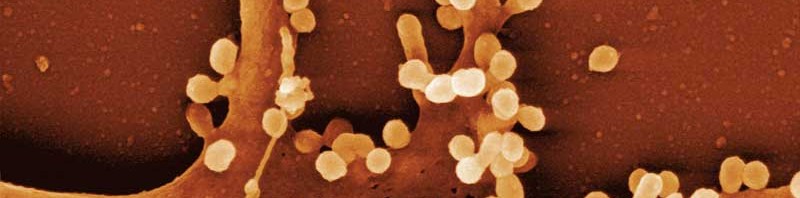
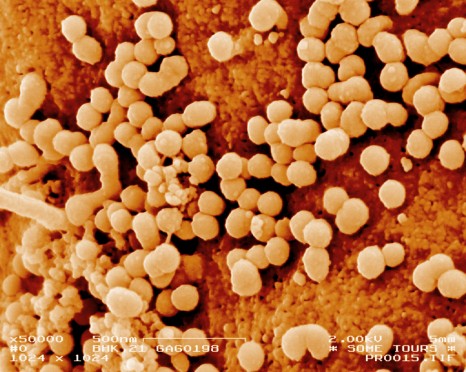
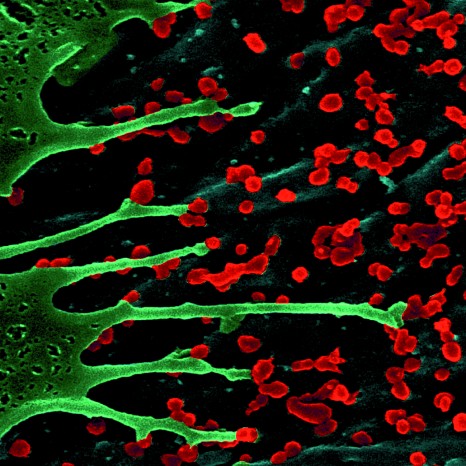
Cyclophosphamide is one of the most widely used drugs in chemotherapy. However, like any treatment, it involves side effects (inflammation of the mucosa etc.), and disrupts the normal balance of the intestinal microbiota. Certain bacteria (of the Gram+ group of bacteria) can pass the intestinal barrier and enter the bloodstream and lymph nodes.
These bacteria, once in the general circulation of the body, may be considered harmful, and the body generates an immune response.
“This chain reaction, a side effect of the treatment, actually turns out to be very useful,” explains Laurence Zitvogel. “Surprisingly, the immune response directed against these bacteria helps the patient to better fight his/her tumour, by stimulating fresh immune defence mechanisms.”
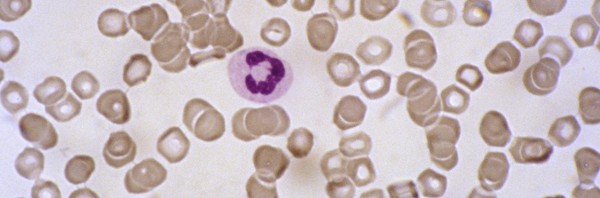
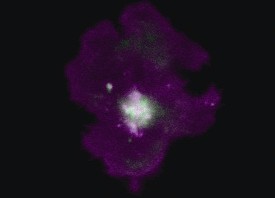
More specifically, immunisation against bacteria leads to the recruitment of effector lymphocytes different to those mobilised by chemotherapy. Their role consists of helping anti-tumour lymphocytes to stem the growth of tumours.
To verify these observations in mice, researchers suppressed all Gram+ bacteria from their intestinal microbiota. Results showed that the efficacy of the chemotherapy was reduced. The researchers also suggest that some antibiotics used during chemotherapy may destroy these Gram+ bacteria, and thus negate their beneficial effect.
“Now that these “beneficial” bacteria that potentiate the anti-tumour immune response have been identified, we should soon succeed in supplying more to the body, especially via pro- or prebiotics and/or a specific diet,” the researcher concludes.