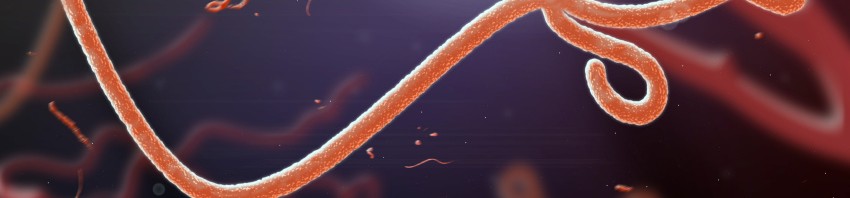
A clinical trial project, coordinated by Inserm, involving the testing of a preventive vaccine against Ebola has been selected by the European Commission. The protocol plans to include participants throughout Europe and Africa to evaluate immune response and tolerance to a vaccine strategy named “prime boost”, based on the use of two candidate vaccines developed by Janssen, a pharmaceutical company of Johnson & Johnson.
The development and rapid access to treatment and candidate vaccines are among the WHO’s recommendations to stop the transmission of the Ebola virus and prevent the international spread of infection. Since the beginning of the epidemic, the French and international scientific community has been actively working towards these objectives.
Inserm has established an academic partnership with the London School of Hygiene and Tropical Medicine (LSHTM), as well as an industrial partnership (Crucell Holland BV; one of Janssen’s companies), The University of Oxford and the Centre Muraz to develop a vaccination from Phase 1 to Phase 3 that combines two vaccines derived from viral vectors (Ad26.ZEBOV et MVA-BN-Filo[1]). This project has been selected for funding by the European Commission under the second call for IMI2 (Innovative Medicines Initiative) projects. As part of this programme, Inserm will conduct Phase 2 trials in Europe and Africa, coordinated by Prof. Rodolphe Thiébaut.
These Phase 2 trials will evaluate the tolerance and quality of the immune response to the vaccine strategy. These tests will supplement data from Phase 1 trials that are currently in progress in the United States, England and are soon to be conducted in Africa. The data will be available in March 2015 and will be critical to evaluating effectiveness in areas at risk.
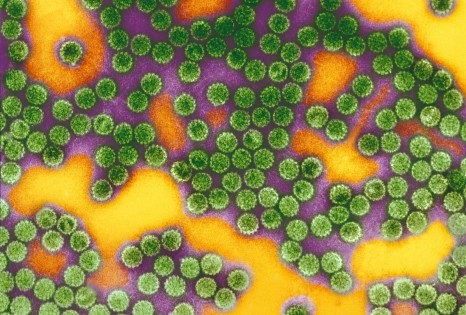
“This strategy, unlike conventional immunization protocols that involve one or more administrations of the same vaccine, is based on the concept of a vaccination involving several steps with two different vectors that will expose the organism to the same antigens in several ways. This is a new approach in the development of a vaccine against Ebola” stated Prof. Yves Levy, Inserm CEO.
The Grant Agreement is currently being finalised. Definitive information on the project, including the budget, will be published once the agreement has been signed.
[1] Both viral vectors used are conventional vectors that are already widely used in humans in several vaccines for other infectious diseases.