The findings of this study are based on records of all deaths having occurred in France over a 49-year period, compiled by the Inserm CépiDc. © Adobe Stock
Temperature and mortality are linked. There is a short-term increase in mortality when temperatures are at their hottest or coldest – a phenomenon known as a “U-shaped relationship”. Inserm researchers at the Institute for Advanced Biosciences (Inserm/Université Grenoble Alpes/CNRS) and the Inserm Epidemiology Center on Medical Causes of Death (CépiDc) have sought to determine the extent to which this relationship between temperature and mortality varies according to the medical cause of death; for what causes of death is the effect of hot temperatures the highest; and whether there are signs of adaptation to extreme temperatures – an important question in the context of climate change. This new study, based on all of the deaths having occurred in France over a 49-year period, confirms the U-shaped relationship (see Graph 1 below) observed between temperature and the majority of the causes of death considered. However, an exception has been observed for death from suicide, which rose steadily in line with the temperature, without the increased risk at cold temperatures observed for the other causes of death. Furthermore, the effect of temperatures at either extreme on all-cause mortality seems to have reduced slightly during this period, which could mean that our society is adapting better. This research has been published in the American Journal of Epidemiology.
Previous scientific publications have studied the short-term link between mortality (irrespective of cause) and temperature – with excess mortality documented during both the hottest and coldest periods, which corresponds to a U-shaped relationship.
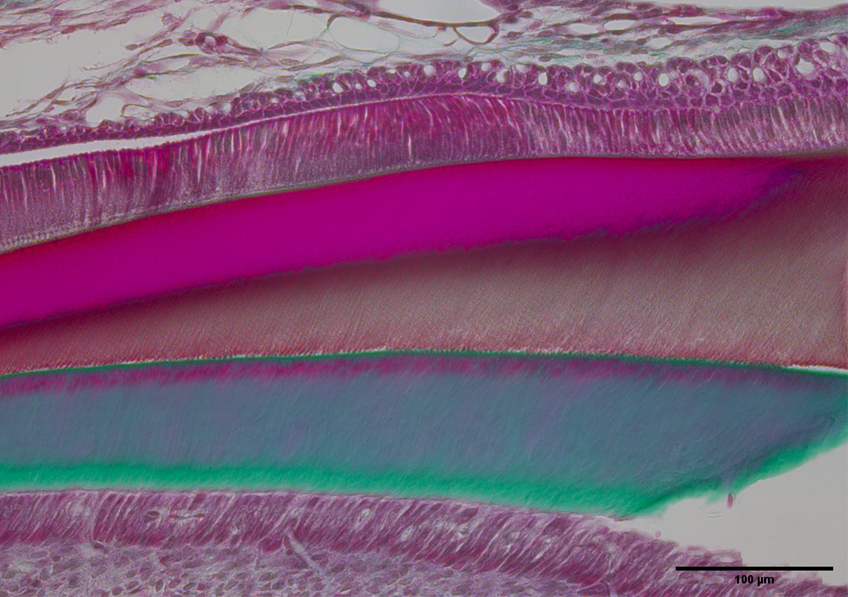
For the first time, Inserm researchers at the Institute for Advanced Biosciences in Grenoble were able to study this phenomenon over a period of almost 50 years and rank the causes of death according to their sensitivity to heat. They based their study on the Inserm medical causes of death (CépiDc) registry, whose records date back to 1968. A total of 24.4 million deaths were recorded over 49 years, including over 502,000 by suicide.
The scientists cross-referenced the number of deaths occurring each day in each region along with daily temperatures throughout the study period. The approach[1] concerned only the short-term links between temperature and mortality, and not long-term trends in mortality or geographic variations in mortality.
“Here we are seeing just one of the last stages of a long and complex multifactorial causal chain leading to death,” explains study leader and Inserm research director, Rémy Slama.
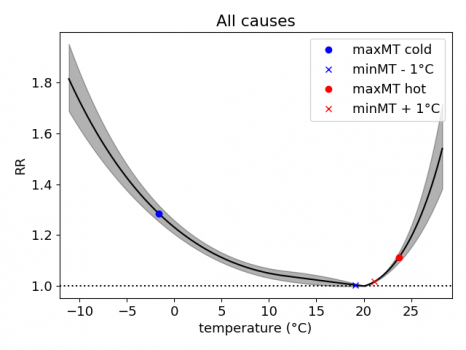
Graph 1: Association between temperature (x-axis) and relative risk of all-cause mortality (y-axis) for the 1968-2016 period (U-shaped relationship)
When all deaths were considered simultaneously, the mortality rate was minimal when the temperature was close to 20°C, and crossed when the temperature either increased above or decreased below 20°C. Among the 22 causes of death considered, almost all followed this U-shaped relationship described in previous studies (see graph above).
Suicide mortality was a notable exception, with a steady increase in line with temperature – from the lowest temperatures to the highest (see graph below). Among the 22 causes of death considered, suicide was ranked seventh place in terms of sensitivity to heat.
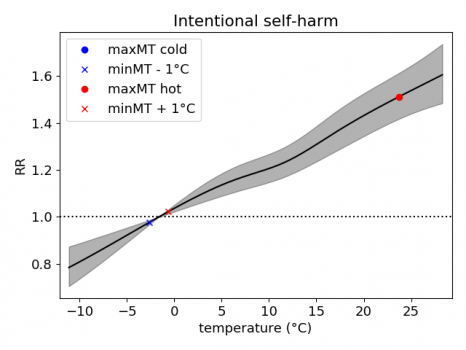
Graph 2: Association between temperature and suicide mortality over the 1968-2016 period
As far as the link between heat and suicide is concerned, the strongest association was found with the temperature on the day of death (rather than that of the preceding days), signifying that it is a very short-term association.
Finally, among the 10 causes of death most strongly related to heat, four involved the nervous system (mental and behavioral disorders, nervous system diseases, cerebrovascular diseases, and suicide). This suggests substantial nervous system sensitivity to high temperatures.
“In order to explore these findings in greater depth, it would be interesting to study the biological parameters that would enable us to understand the underlying mechanisms behind this link between temperature and suicide,” explains Slama.
“The existing hypotheses include at least two non-exclusive avenues: one being the changes in social relationships when temperatures are very high, which could influence suicide; the other being an alteration in endocrine and nervous system functioning in the event of extreme heat, which could increase the risk of suicide, he continues. Research shows that levels of the hormone serotonin tend to decrease when temperatures are high. However, lower levels of this neurotransmitter, which is involved in regulating mood and anxiety, could play a role in the decision to commit suicide,” concludes the research director.
Tendency of French society to adapt to extreme temperatures
The relative wealth of data offered by the registry of the causes of death also made it possible to study the question of adaptation to extreme temperatures. By dividing the study period into three, the scientists were able to study whether the effect of temperatures varied between these periods.
The effects of temperature on all-cause mortality and suicide mortality were attenuated between the 1968-1984 and 1985-2000 periods: for a given temperature, the risk of death was lower during the 1985-2000 period than during the 1968-1984 period. This was seen both for hot temperatures above 20°C and cold temperatures of around 0°C. However, no further attenuation was observed during the 2001-2016 period compared to the previous period (1985-2000).
These findings show the tendency of French society to adjust to extreme temperatures – hot and probably also cold – at the end of the 20th century.
“Although it was not the objective of the study to explain the drivers of this adaptation, we can hypothesize that it is essentially societal, involving improvements to housing and the health system rather than the result of biological evolution, which in principle is very slow,” explains Slama.
The short-term association between temperature and suicide risk could be taken into account in prevention campaigns related to the effects of heat and suicide. It also raises the question of the expected impact of climate change on mortality, which particularly depends on the relationship between temperature and mortality and the ability of societies to adapt to extreme temperatures.
[1] Known as a “time series” analysis
If you are having suicidal thoughts, call 3114. The national suicide prevention number is open 24/7. Free and confidential, professionals are there to listen to you.