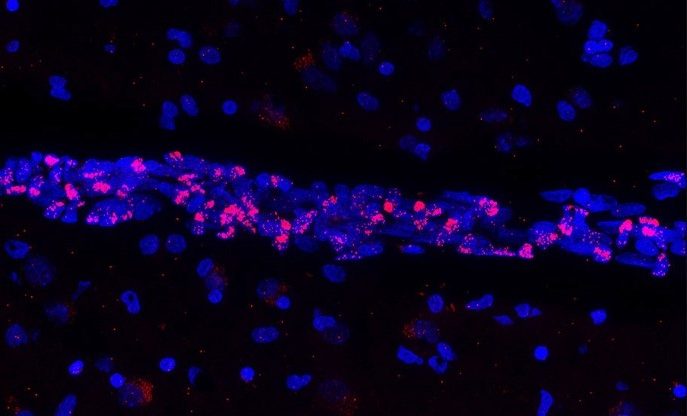
The patients who best respond to the dual therapy in this study have a “Mitoscore signature” associated with strong mitochondrial activity. © Adobe Stock
While the care and treatment of acute myeloid leukemia (AML) have greatly improved in recent years, overall survival remains low. Resistance to the various treatments continues to present a major clinical challenge. Using animal models, and also by working with patients themselves, scientists from Inserm, CNRS and Université Toulouse III – Paul Sabatier at the Cancer Research Center of Toulouse have identified a new biomarker predictive of response to dual therapy (chemotherapy plus targeted therapy) used in AML, as well as resistance mechanisms behind relapses. The findings of this research have been published in Nature Cancer.
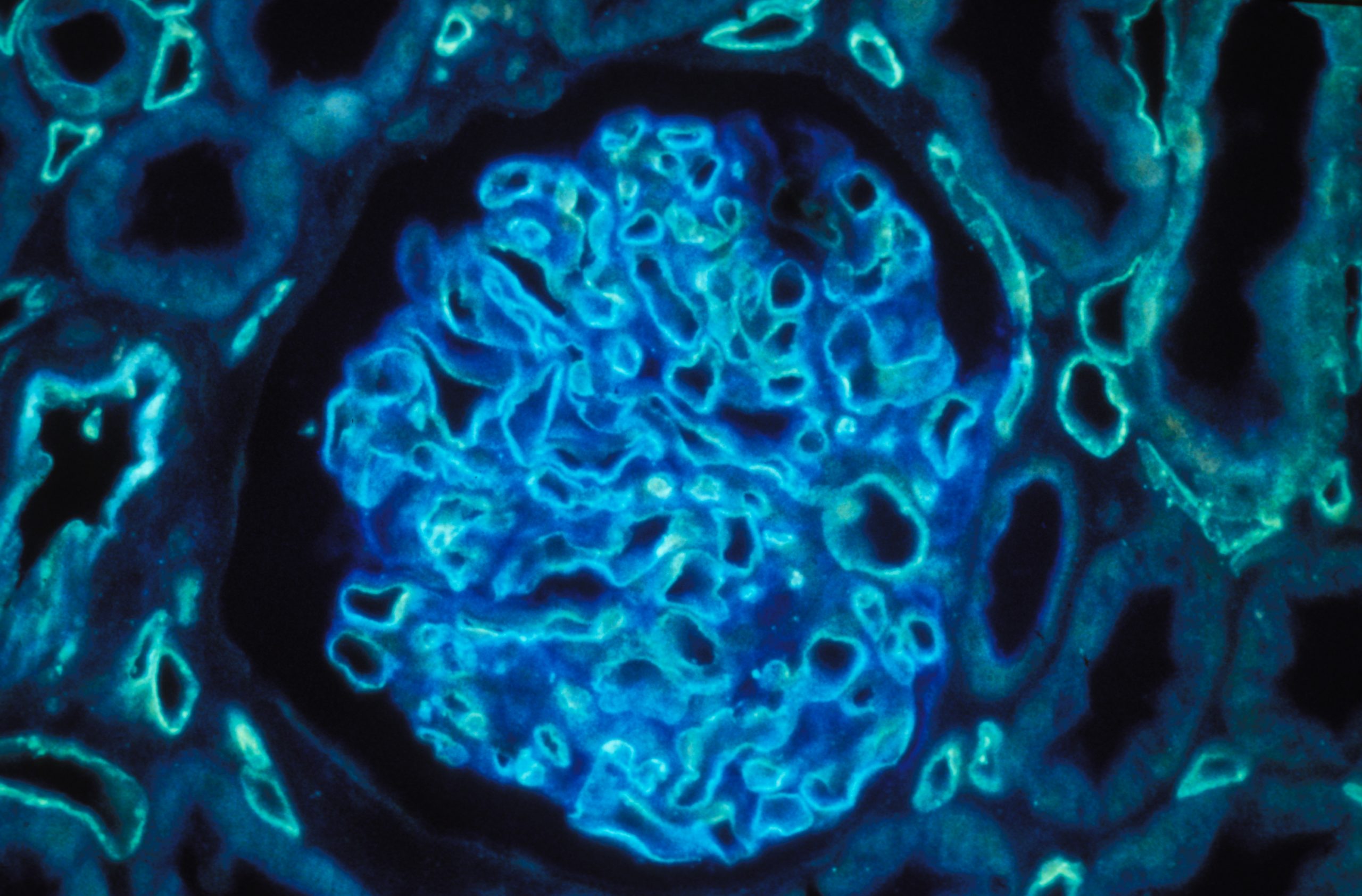
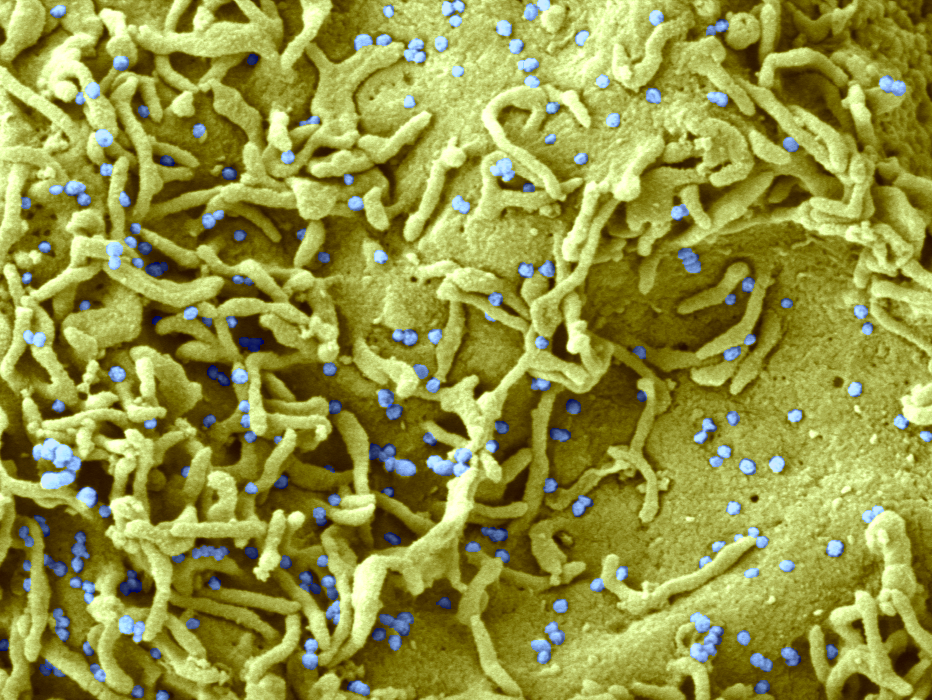
Leukemia groups several types of blood cancer that affect nearly 10,000 people each year in France. These include acute myeloid leukemia (AML), which affects the hematopoietic cells[1] in the bone marrow.
For a long time, intensive chemotherapy has been the treatment of choice for patients. Although the majority respond favorably and go into remission, overall survival in the longer term remains low, with certain resistant cancer cells persisting in the body following chemotherapy and leading to relapse.
In recent years, the development of targeted therapies has improved the treatment and response of patients, prolonging survival a little – particularly in elderly people ineligible for chemotherapy. However, even with these therapies, relapse remains a major issue. Understanding the mechanisms underlying resistance to leukemia treatments and finding a way to resolve them are a central focus of the work of Inserm researcher Jean-Emmanuel Sarry and his team at the Cancer Research Center of Toulouse (Inserm/CNRS/Université de Toulouse III – Paul Sabatier).
While most scientists working on the subject are more interested in the genetic mechanisms associated with resistance, Sarry’s team is studying the non-genetic mechanisms in order to understand why some patients are more likely to relapse.
Identification of a “Mitoscore signature”
In their new study, the researchers looked at a recently approved dual therapy (conventional chemotherapy combined with a new targeted therapy), which is increasingly used in the treatment of AML.
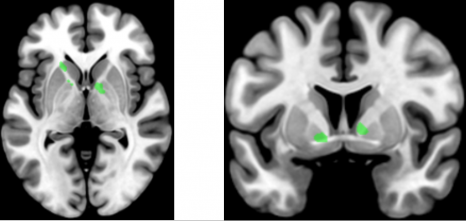
Using patient transcriptomes (i.e. all messenger RNA derived from genome expression), they show that people who respond best to the dual therapy and who have prolonged survival have a specific biomarker – a “Mitoscore signature” – that is associated with a high level of mitochondrial activity[2]. “In other words, this strong Mitoscore signature, which reflects a high level of mitochondrial activity, is predictive of an improved response to these treatments,” explains Sarry.
Finally, thanks to single-cell sequencing[3]of residual disease[4] following this dual therapy, the researchers observed a particular remodeling of mitochondrial function allowing cancer cells to adapt to therapies and induce the patient’s relapse. In mice, the team also showed that treatment based on a molecule that inhibits the action of the mitochondria makes it possible to block this mitochondrial function remodeling, prevent relapse, and prolong the animals’ survival.
“The objective is now to test this Mitoscore signature on very large cohorts in order to validate its utility. Ultimately, the idea would be to use this biomarker to improve patient follow-up and offer more personalized therapies – by giving dual therapy, possibly also with the mitochondrial inhibitor, for those likely to benefit from it. This research could therefore have a real clinical impact in the years to come,” explains Sarry.
1 Hematopoietic stem cells are made by the bone marrow and develop into the various blood cells: red cells, white cells, and platelets. Source INCa
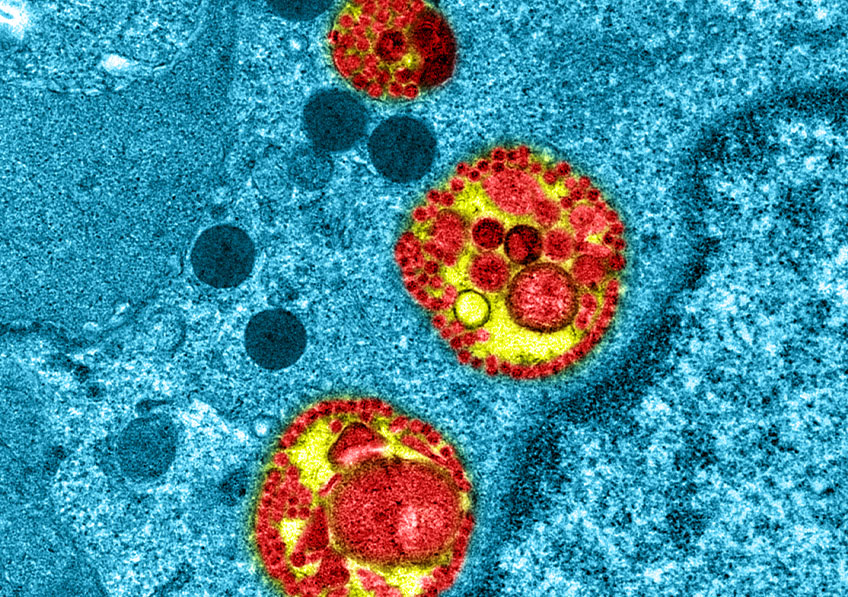
2 Mitochondria are intracellular organelles whose role is to provide the cells with the energy they need. They therefore play a central role in cellular energy metabolism.
3 Single-cell sequencing is a set of molecular biology techniques used to analyze genetic information at single-cell level, using next generation sequencing technologies.
4 Residual disease is the persistence in tissue of malignant cells below the detection limit of conventional techniques.