Between 1966 and 1974, France performed 41 atmospheric nuclear tests in French Polynesia. © Unsplash
The health outcomes of the nuclear tests performed in French Polynesia in the 1970s have been the subject of epidemiological studies at Inserm for several years. Previous research published by a team from Inserm and Université Paris-Saclay with the Gustave-Roussy Institute had studied the relationship between the frequency of thyroid cancer in French Polynesia and the atmospheric nuclear tests performed by France. It had found a very probable slight increase in the thyroid cancer risk with the radiation dose received following the nuclear tests. In a new publication, the scientists confirm these findings and conduct a risk prediction analysis showing that these nuclear tests could be responsible for 2.3% of the thyroid cancer cases. The particularity of this study, whose results have been published in JAMA Network Open, lies in the access to the original internal reports by the radiation-protection services that relate to 41 atmospheric nuclear tests performed by France between 1966 and 1974 in French Polynesia, declassified by the French military in 2013.
Between 1966 and 1974, France conducted 41 atmospheric nuclear tests in Polynesia. For several years, research teams have attempted to evaluate the potential consequences of the radioactive fallout on population health. They have particularly focused on diseases that may be radiation-induced, such as cancer, cardiovascular diseases, and cataracts.
In an Inserm Collective Expert Review produced in 2021 (only available in French), researchers mentioned two epidemiological studies published on the subject, one of which concerns the risk of developing thyroid cancer. Due to the amount of radioactive iodine released in nuclear tests and its active absorption by the thyroid, this form of cancer is the most serious health risk for the population living near the nuclear test sites.
This is because when radioactive iodine binds to the thyroid instead of natural iodine, it exposes the gland to the radiation it emits. If high levels of this radioelement are found in the thyroid, this radiation may damage the DNA and lead to the development of cancerous tumors.
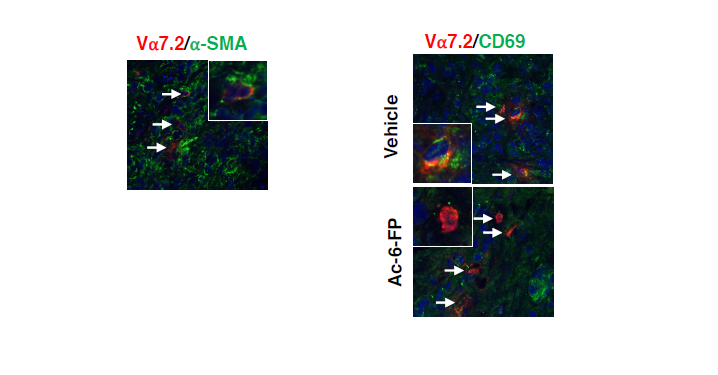
In a study published in 2010 in the British Journal of Cancer, researchers from Inserm and Université Paris-Saclay at the Center for Research in Epidemiology and Population Health (CESP) at the Gustave-Roussy Institute compared the radiation exposures of 229 Polynesians diagnosed with differentiated thyroid carcinoma between 1981 and 2003 with those of 373 “control” individuals who had not developed thyroid cancer in the same population. This case-control study conducted in the local population had shown a small increase in the risk of thyroid cancer in line with an increase in the dose received by the thyroid before the age of 15.
Although these findings are insufficient in providing a firm conclusion on the links between the fallout of the atmospheric nuclear tests and the occurrence of radiation-induced diseases in French Polynesia, they also did not rule out the existence of health impacts.
Continuing this research, the same team conducted a second epidemiological study, this time on 395 cases of thyroid cancer diagnosed between 1984 and 2016 in Polynesia and 555 controls from the general population. For the first time, they had access to the original radiation-protection service reports relating to the 41 atmospheric nuclear tests performed by France between 1966 and 1974 in French Polynesia, declassified by the French military in 2013.
Thanks to these declassified documents, meteorological data, and interviews with cases and controls (population movements, dietary habits, etc.), the researchers were able to simulate the radioactive cloud of each nuclear test and estimate the dose of radiation received to the thyroid of the study participants. This was on average 4.7 milligray for the cases and 4.6 milligray for the controls.
For all of the cancer cases (395 people), the scientists did not find a significant association between the dose of radiation received by the thyroid and the risk of thyroid cancer. However, the relationship was significant if the analysis only considered the invasive cancers requiring treatment, and excluded the noninvasive microcarcinomas that are common and usually do not need surgery.
Using these cross-referenced data (population movements, dietary habits and rates of thyroid cancer incidence), the researchers also made a risk prediction and showed that, based on current risk models, the nuclear tests performed by France could be responsible for a total of 2.3% of all thyroid cancer cases (confidence interval between 0.6 and 7.7%[1]).
“These findings are consistent with our previous conclusions and confirm that the nuclear tests are most likely responsible for a small increase in the incidence of thyroid cancers in French Polynesia. However, these findings should be considered with caution as the estimated radiation doses received by the thyroid over 50 years ago are bound to be inaccurate,” explains Florent de Vathaire, Inserm researcher at Gustave-Roussy, and first author of the study.
The scientists are continuing their research with the aim of adding to their analysis the evaluation of the genetic susceptibilities of the populations (hereditary factors and genetic combination specific to each individual) that could affect the development of thyroid cancers in the region.
[1] The confidence interval defines a minimum and maximum value between which, for a given risk of error, the exact value of the entire population is situated.