Vaccination Covid-19 et populations particulières : une grande étude de cohorte pour orienter les recommandations destinées aux plus fragiles



The appendix is an anatomical structure that can be found in a wide range of very different species, from the orangutan to the koala, beaver, and of course humans. © 
Long considered an unnecessary organ, the appendix is now the focus of several studies that aim to better understand its role. Present in many mammals, including humans, it appears to have developed at least 16 times over the course of the evolutionary history of mammals, suggesting that its function must confer a positive selective advantage on those that have it. A new study carried out by researchers from Inserm and the French Museum of Natural History suggests that the presence of the appendix is in fact correlated with greater longevity. Their findings have been published in the Journal of Anatomy.
The appendix is a small anatomical structure of a few centimeters in size, located in the abdomen and attached to the colon, the function of which has long been poorly understood. According to the theories of Charles Darwin, the appendix was a vestigial structure, useless and devoid of function. It might even be seen as potentially dangerous to health due to the risk of inflammation of the organ. If such inflammation, known as “appendicitis,” is left untreated, it can develop into peritonitis and result in death.
Over the last few years, researchers have sought to learn more about the role of the appendix. Studies have, for example, shown that an appendectomy performed in cases of confirmed appendicitis before the age of 20 has a protective effect against the onset of a particular form of chronic inflammation of the colon and rectum: ulcerative colitis.
Researchers have also shown that the appendix is not only present in humans. It first appeared in mammals at least 80 million years ago, and over the course of evolution has developed independently multiple times in several mammalian lineages, with no obvious correlation with diet, social life, or the environment. Today it can be found in a wide range of animals: from orangutans and koalas to manatees, beavers, and platypuses. Its function has however remained a mystery, with no study reaching a definitive conclusion.
The team led by Inserm researcher Eric Ogier-Denis and his colleague Michel Laurin from the French Museum of Natural History approached the question by analyzing data from 258 species of mammals, 39 with and 219 without an appendix. The scientists focused in particular on the theoretical maximum longevity (the theoretical lifespan of mammals, established based on their weight) and actual maximum longevity of the various species considered.
“The idea of focusing on longevity developed from our work on the relationship between appendicitis/appendectomy, ulcerative colitis and the involvement of the immune system. A more active and better educated immune system should theoretically provide greater resistance to the environment and a longer lifespan. We therefore tested this hypothesis by partnering with two internationally renowned evolutionary experts from the French Museum of Natural History. This is the first time the existence of a correlation between the presence of the appendix and a trait in the life history of mammals has been demonstrated,” explains Eric Ogier-Denis.
The team has also shown that the appendix has developed at least 16 times and has only been lost once (by the lemur Hapalemur griseus, endemic to Madagascar) during the evolutionary history of mammals, which supports the idea that
through its function this organ provides a significant positive selective advantage with regard to the laws of natural selection.
The researchers believe that the most likely hypothesis to explain the link between the presence of the appendix and longevity is that the shape of the organ enables the development of a selective “bacterial sanctuary” that reduces mortality from infectious diarrhea by promoting rapid recolonization of bacterial species that are essential to the host. The presence of the appendix would therefore be associated with a decrease in mortality and thus greater longevity in mammals that have this organ.
“This does not mean that an appendectomy performed on a human to treat appendicitis has an effect on longevity. Appendicitis at a young age is clearly beneficial by strengthening the education of the immune system and enabling it to fight any subsequent infection more effectively. The treatment for appendicitis remains appendectomy and this work does not provide any evidence to suggest this treatment approach should be changed. Only an appendectomy performed in a patient without appendicitis might have harmful consequences in the context of inflammatory and infectious bowel disease,” explains Eric Ogier Denis.
This work therefore opens up clear new avenues of research for elucidating the controversial issue of the function of the appendix. Over the coming months, the researchers will build on it with field studies looking at different species of mammals to confirm the link between the appendix and longevity.
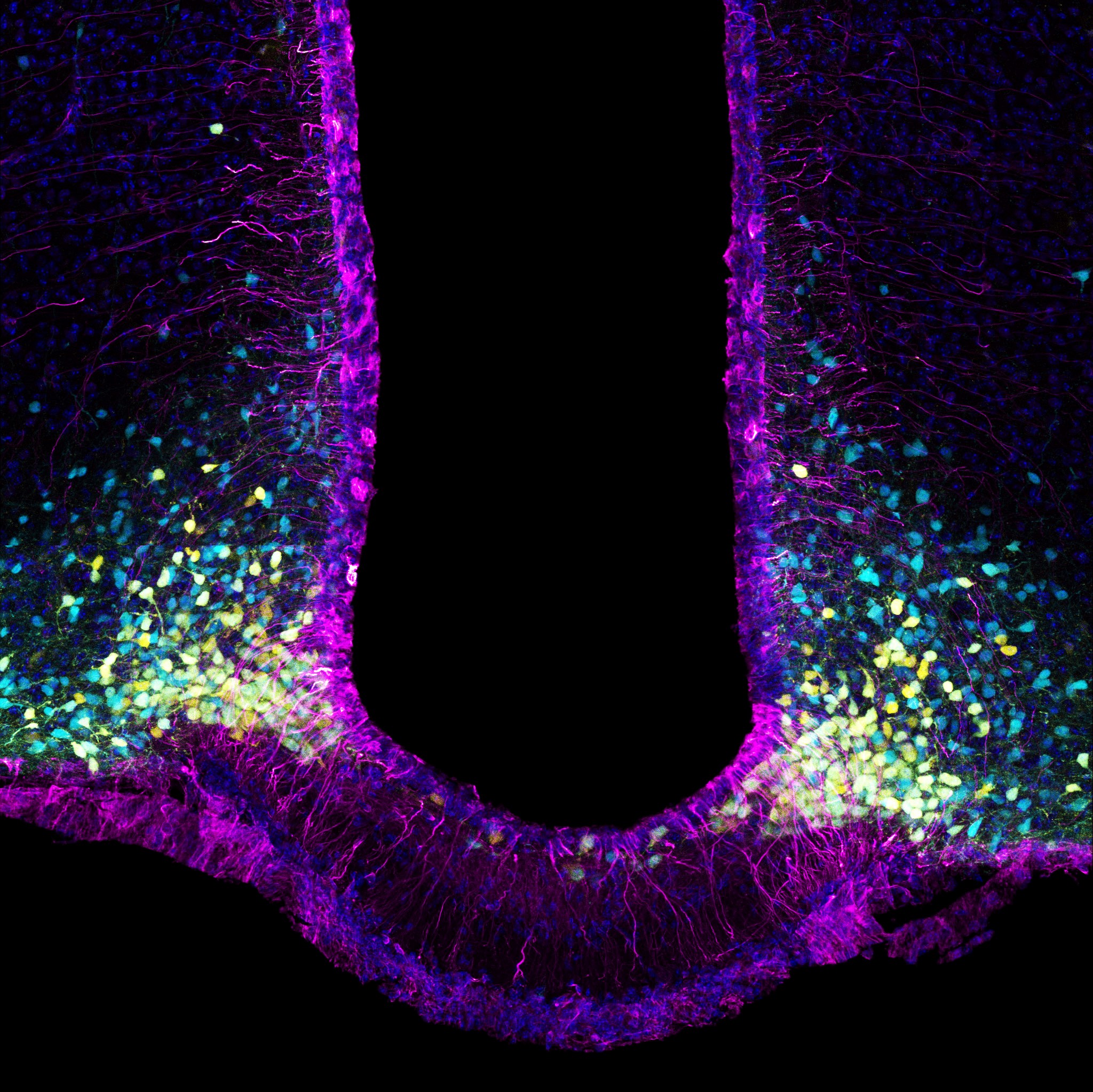
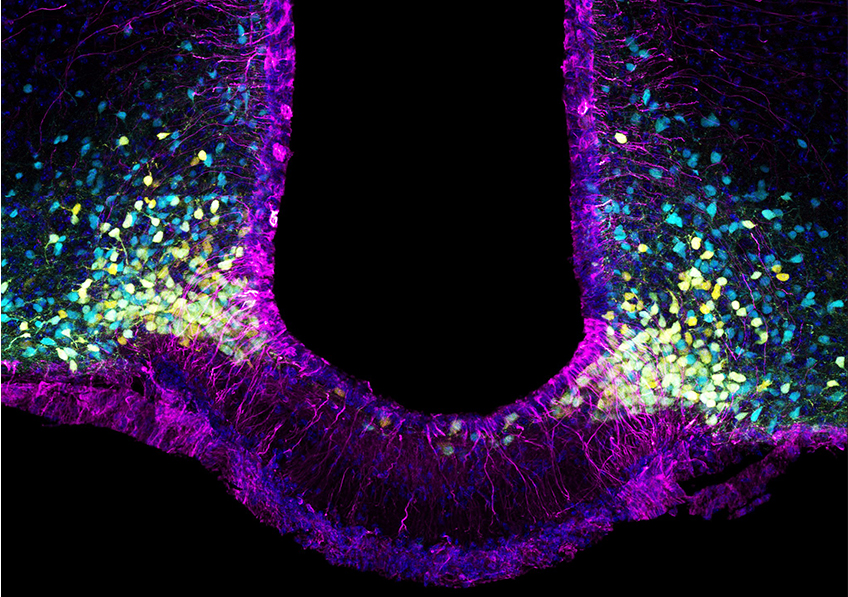
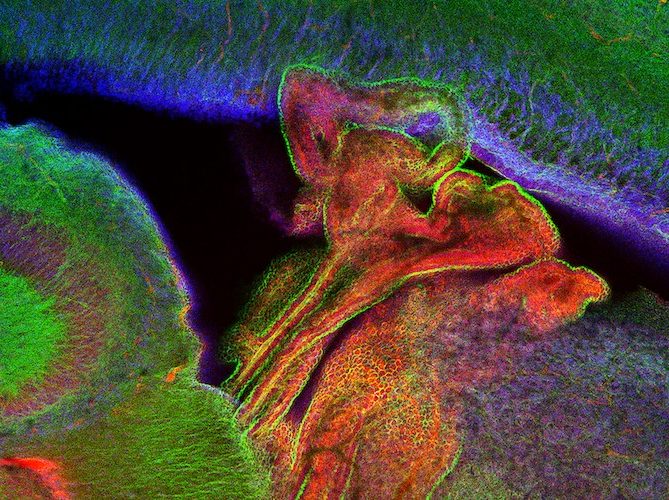
In purple, the tanycytes that form the brain’s cellular gateway to the hormone leptin; in yellow, the appetite-inducing neurons and, in blue, the appetite-suppressing neurons. Leptin targets both neuron types, inhibiting the former and using its appetite-suppressant signal to activate the latter. © Vincent Prévot
Diabetes, a disease in which blood sugar levels remain too high for too long, can lead to health complications in the long term. Type 2 diabetes (T2D) accounts for 90% of cases. Patients are usually obese or overweight, with risk factors that include sedentary lifestyle and unbalanced diet. To increase their understanding of the disease, a team of researchers from Inserm, Université de Lille, and Lille University Hospital in the Lille Neuroscience and Cognition laboratory[1] has for several years studied the role of leptin, a hormone involved in appetite control that sends satiety signals to the brain. In a new study published in the journal Nature Metabolism, in addition to furthering scientific knowledge of the mechanism of satiety, the scientists developed a new mouse model of diabetes that will be useful for and relevant to future research in this area.
Leptin, the satiety or appetite-suppressant hormone, is secreted by the adipose tissue at levels proportional to the body’s fat reserves and regulates appetite by controlling the feeling of fullness. It is transported to the brain by tanycytes – cells which it enters by attaching to the LepR receptors. Tanycytes are therefore leptin’s gateway to the brain, helping it to cross the blood-brain barrier and deliver satiety information to the neurons.
Previous research has revealed that such transport is impaired in subjects who are obese or overweight. This goes some way to explaining their dysfunctional appetite regulation given that it is more difficult for the information on satiety to reach the brain. In their new study, the researchers took a closer look at this transport mechanism, and more precisely the role played by the LepR receptors.
The key role of satiety hormone receptors in glucose management
In mouse models, the researchers removed the LepR receptor that is located on the surface of the tanycytes. After three months, the mice experienced a marked increase in their fat mass (which doubled over the period) as well as a loss of muscle mass (reduced by more than half). The total amount of weight gained was only fairly moderate. The scientists also regularly measured the animals’ blood sugar levels following the injection of glucose.
They found that in order to maintain blood sugar at normal levels (between 0.70 and 1.10 g/L), the mice secreted more insulin during the first four weeks of the experiment. Three months after removing the receptor, their ability to secrete insulin from the pancreas appeared to be exhausted.
Removing the LepR receptors and impairing leptin transport to the brain therefore led the mice to initially develop a pre-diabetic state. This occurs when the body releases more insulin than usual in order to control blood sugar. Then, in the longer term, the mice became unable to secrete insulin and as such unable to control their blood sugar levels. These data therefore suggest that impaired leptin transport to the brain via the LepR receptors plays a role in the development of type 2 diabetes.
In a healthy animal or person, blood sugar levels rise slightly after the ingestion of glucose and then decrease rapidly. In order to bring blood sugar back to within normal limits, the pancreas secretes insulin that helps the glucose to penetrate the body’s cells.
In animals deprived of the LepR receptor where leptin enters the brain, blood sugar levels are abnormally high in the fasting state and even more so after ingesting glucose. The pancreas becomes unable to secrete the insulin needed for the body to absorb the glucose. The brain’s “deafness” to the information conveyed by leptin thereby renders the pancreas ineffective.
In the last part of their research, the scientists reintroduced leptin to the brain and observed the immediate resumption of its pancreatic function-promoting action – particularly the ability of the pancreas to secrete insulin to regulate blood sugar. The mice quickly regained a healthy metabolism.
This study therefore elucidates the brain’s role in type 2 diabetes and also helps to further research into a disease that until then had not been considered to involve the central nervous system.
“We show that the brain’s perception of leptin is essential for the management of energy homeostasis[2] and blood sugar. We also show that blocking the transport of leptin to the brain impairs the functioning of the neurons that control pancreatic insulin secretion,” concludes Vincent Prévot, research director at Inserm and last author of the study.
Another interesting finding of this study: by removing the LepR receptor where leptin enters the brain, the animal model obtained exhibits the characteristics of so-called East Asian Diabetes, still little studied by researchers. This diabetes phenotype mainly affects the populations of Korea and Japan.
While so-called Western Diabetes is mainly associated with people who are markedly overweight (BMI >25) or morbidly obese (BMI >30), this other type 2 diabetes phenotype is often associated with people who are slightly overweight, have increased levels of abdominal fat, and insulin insufficiency related to deficient insulin secretion by the pancreas.
According to the scientists, the development of this new animal model will make it possible to further research into this disease that affects millions of people.
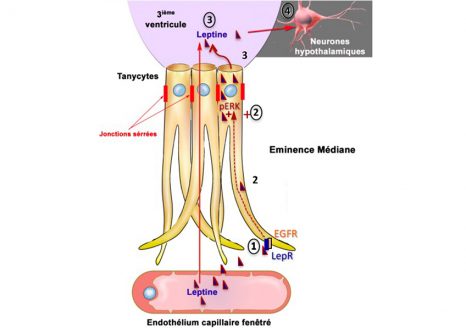
The research team started by describing the mechanism by which leptin passes through the cell gate: tanycytes (Figure opposite: cells in yellow). These cells capture circulating leptin from the blood vessels which at that location have the particularity of letting it through (step 1). Whilst in the tanycyte, the leptin captured by LepR activates the EGF receptor (or EGFR) which itself activates an ERK signaling pathway (step 2), triggering its release into the cerebrospinal fluid (step 3). The leptin then activates the brain regions that convey its anorectic (appetite suppressant) action, as well as control of pancreatic function (step 4).
[1] This research was performed in collaboration with two laboratories at Institut Cochin and Université de Strasbourg as part of a project funded by the French National Research Agency (ANR) and two European laboratories, one at Lübeck University in Germany and the other at the University of Santiago de Compostela in Spain, within the framework of European Community funding. In addition, the Lille Neuroscience and Cognition laboratory is a member of LabEx EGID (European Genomic Institute for Diabetes) and DISTALZ (Development of Innovative Strategies for a Transdisciplinary approach to ALZheimer’s disease).
[2] Stabilization, regulation in living organisms, of certain physiological characteristics (food intake, energy expenditure, etc.).


The under 6 year-olds are the category of children most exposed to drug prescriptions. © Myriam Zilles – Unsplash
France is one of the countries with the highest levels of drug consumption in Europe. In the absence of updated data from the last ten years on pediatric drug prescriptions, researchers from Inserm and teacher-researchers from Université de Paris at the Center for Research in Epidemiology and Statistics (CRESS), along with researchers from Université de Versailles Saint-Quentin-en-Yvelines / Université Paris-Saclay, the Paris hospitals group AP-HP, and the Epi-Phare scientific interest group, quantified pediatric outpatient prescriptions in France and studied their evolution between 2010 and 2019. Their findings have been published in The Lancet Regional Health Europe.
The pediatric population, especially very young children, is particularly vulnerable to the short and long-term side effects of drugs because of its immaturity. In addition, the safety profile of many drugs used in pediatrics is only partially known. These elements should encourage rational prescribing in this population.
The first French national study of drug prescriptions in pediatric outpatient populations, based on data from the Generalist Sample of Health Insurance Beneficiaries (EGB) from 2011, showed worrying results with the highest frequency of prescriptions in the world. However, since 2011, new recommendations on the proper use of certain drugs have been issued and reimbursement delisting policies have been implemented, which were expected to lead to changes in these prescriptions.
The objective of the new study, conducted by researchers and teacher-researchers from Inserm, Université de Paris, Université de Versailles Saint-Quentin-en-Yvelines / Université Paris-Saclay, the Paris hospitals group AP-HP, and the Epi-Phare scientific interest group (GIS), was to determine the frequencies of drug prescriptions in pediatric outpatients in 2018-2019 in France and to compare them with those of 2010-2011, at the national level, using French National Health Data System (SNDS)2 data.
The analysis covered all reimbursed dispensations of drugs prescribed in an outpatient setting (so excluding those prescribed during stays in hospital), by a doctor, midwife or dentist, and intended for all children under 18 years of age living in France. In order to take into account the influence of infectious epidemics on outpatient prescriptions, annual drug prescription frequencies were averaged over two years for the two study periods. For the 2018-2019 period, over 230 million dispensed prescriptions were analyzed.
Children under 6 years of age are the category most exposed to drug prescriptions
The study found that over the recent period (2018-2019), on average, 86 out of every 100 children under 18 years of age had been exposed to at least one drug prescription over the course of one year, representing a 4% increase in relation to 2010-2011. Children under six years of age were the category most exposed to drugs, with over 97 out of every 100 children affected in a year.
The most prescribed therapeutic classes for the 2018-2019 period were analgesics (64%3), antibiotics (40%), nasal corticosteroids (33%), vitamin D (30%), nonsteroidal anti-inflammatory drugs (24%), antihistamines (25%), and oral corticosteroids (21%).
“Following the publication of the 2011 data, we expected to see a significant change for certain therapeutic classes given the regulations put in place or recommendations issued since 2011. A 12% decrease in the frequency of antibiotic prescriptions over the past ten years was noted in our study, but this remains insufficient because more than one in two children under 6 years of age were prescribed antibiotics during the year,” explains Dr. Marion Taine, co-author of the study.
Finally, 2% of infants under 6 weeks of age were prescribed proton pump inhibitors4 during the year 2018-2019, “even though the frequency of conditions for which this treatment is recommended is much lower at this age,” explains Dr. Taine.
France, one of the highest prescribing countries for outpatient pediatric drugs
France is one of the countries that prescribes the most drugs in outpatient pediatrics, but international comparisons need to be treated with caution given that health care systems and drug reimbursement policies (particularly for those available over the counter) differ from country to country.
For example, comparisons between a few advanced-economy countries show that the frequencies of oral corticosteroid prescriptions for French children were 5 and 20 times higher than those observed for American and Norwegian children in other recent studies. For antibiotics, the frequency of prescriptions to French children was 5 times higher than that observed in the Netherlands. The inappropriate prescription of antibiotics increases bacterial resistance. As for systemic corticosteroids, their side effects are well-documented.
“These worrying results require in-depth analysis in order to better target future educational campaigns to optimize pediatric medication use. Better information for the population and prescribers regarding the use of medicines in children is essential”, concludes Dr. Taine.
1 Benard-Laribiere A, Jove J, Lassalle R, Robinson P, Droz-Perroteau C, Noize P. Drug use in French children: a population-based study. Arch Dis Child 2015;100 (10):960–5.
2 The SNDS covers 98.8% of the French population and compiles reimbursement data for outpatient care for all children covered by the Universal Public Health Insurance in France
3 643 out of every 100 children received at least one prescription for pain medication over one year on average during the 2018-2019 period.
4 Medications recommended only for complications of gastroesophageal reflux disease.
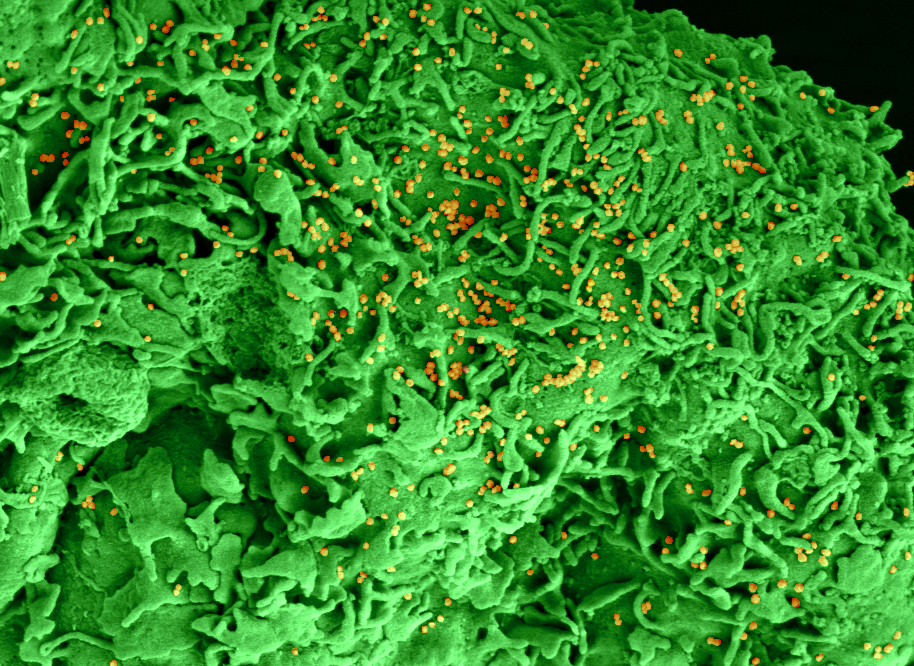
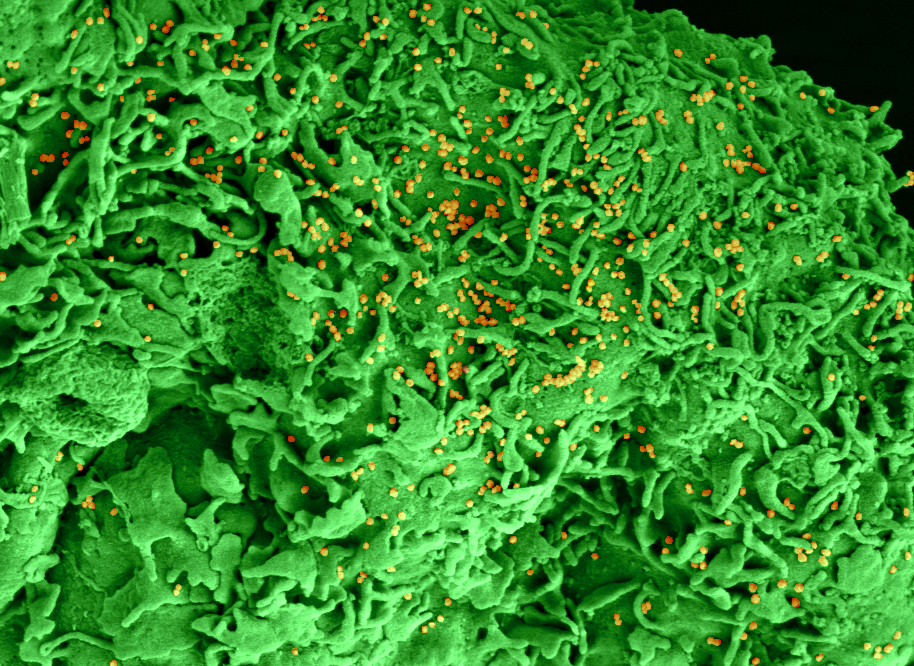
Electronic microscopy of a cell infected with SARS-CoV-2 © Philippe Roingeard, Anne Bull-Maurer, Sonia Georgeault, unité Inserm U1259 MAVIVH & Université de Tours, France
An article published in JAMA Internal Medicine and WHO meta-analysis of 27 controlled trials confirm the promising initial results of the test-CORIMUNO TOCI-1, indicating an improved prognosis of patients with moderate to severe COVID-19 pneumonia. This trial was conducted by the COVID-19 academic research collaboration Assistance Publique-Hôpitaux de Paris / Université Paris-Saclay / Université de Paris / INSERM-REACTing. They reveal the clinical efficacy of tocilizumab, a monoclonal antibody which blocks the receptor for the cytokine interleukin-6 (IL-6) and which is used in particular in the treatment of rheumatoid arthritis.
The 90-day results of the CORIMUNO-TOCI-1 trial published on May 24, 2021 in the journal JAMA Internal Medicine show an improvement in the survival of patients with moderate to severe COVID-19 pneumonia with tocilizumab in highly inflammatory patients .
In some patients with COVID-19 pneumonia, an immune-mediated hyperinflammatory condition contributes to acute respiratory failure and death. The CORIMUNO-19 platform was quickly set up in March 2020 to test the efficacy and safety of various immunomodulatory drugs in adult patients with moderate, severe or critical COVID-19 pneumonia, thanks to a series of ‘multicenter randomized controlled trials, which began on March 27, 2020 and are currently continuing.
Tocilizumab is a monoclonal antibody that blocks the cytokine interleukin-6 (IL-6) receptor.
The CORIMUNO-TOCI-1 randomized trial that compared tocilizumab with the usual treatment, published on October 20, 2020 in the journal JAMA Internal Medicine with a 28-day follow-up , demonstrated that tocilizumab had a 95% chance of reducing the need for ventilation (mechanical or non-invasive) or death at D + 14 (Hazard ratio (HR) = 0.58 (0.33-1.00), but did not decrease mortality at D + 28 (11% and 12%, respectively).
The new update results of this study published on May 24, 2021 in the same journal JAMA Internal Medicine concern longer-term survival (D + 90) and according to the inflammatory state of the patient, in particular according to a threshold of C reactive protein (CRP) (150 mg / L) at the start of treatment.
Mortality at D + 90, a secondary endpoint of the trial, is numerically but not significantly lower in the treated group (11% vs. 18%; HR = 0.64 [0.25-1.65]. A post-hoc analysis shows an interaction between survival and CRP level with, in the group of patients whose CRP is> 150 mg / L, a reduction in mortality with tocilizumab (9% versus 35%; HR = 0.18 [0.04 to 0.89]. the CRP is <or = at 150, the mortality is very low in the 2 treatment groups.
These results obtained on secondary endpoints and in post-hoc analysis had to be confirmed by additional studies and a meta-analysis of all the controlled trials. This is what was done by a group of WHO researchers.
U do the WHO meta-analysis of 27 controlled trials evaluating inhibitors of IL-6 in patients hospitalized for pneumonia Covid-19 confirms a profit of these drugs on survival . It was published in JAMA on July 6, 2021 .
A meta-analysis was carried out by the WHO on all the randomized trials that evaluated inhibitors of IL-6 or its receptor in patients hospitalized with COVID-19 pneumonia requiring oxygen or ventilation. non-invasive or mechanical.
In this prospective meta-analysis of 27 randomized trials (including 4 trials from the CORIMUNO platform) that included 11,112 patients, 2,565 of whom died, 28-day mortality and progression to invasive mechanical ventilation or death were lower in patients who received interleukin-6 antagonists compared to those who received usual care or a placebo (OR = 0.86 [95% CI, 0.79-0.95]; P = 0.03 and OR = 0.77 (95% CI, 0.70-0.85, P <0.001) respectively).
For the 19 trials that evaluated the effect of tocilizumab, the effect on 28-day mortality and progression to invasive mechanical ventilation or death was 0.83 (95% CI, 0.74-0.92; P <0.001 and 0.74, respectively) (95% CI, 0.66-0.82).
In this meta-analysis, tocilizumab did not cause more secondary infections than usual treatment.
In total, these two articles confirm the promising initial results of the CORIMUNO-TOCI-1 and RECOVERY trials.
One of the important questions that remains unanswered is: “Should IL-6 receptor inhibitors replace the standard treatment of these patients which has now become corticosteroid therapy or be added to it?” “.
The CORIMUNO-TOCIDEX protocol which compares dexamethasone alone to the combination of dexamethasone with tocilizumab and which included more than 450 patients is currently attempting to answer this important question.
WHO is due to make recommendations soon on the use of tocilizumab in the different subgroups of patients hospitalized for COVID-19 pneumonia. The FDA announced on June 24, 2021 an emergency authorization for the use of tocilizumab in severe coronavirus lung disease.
Coordinating investigator: Prof. O. Hermine, Hôpital Necker, AP-HP, Imagine Institute, INSERM U1163, University of Paris
Co-coordinating investigator: Prof. X. Mariette, Bicêtre Hospital, AP-HP, INSERM U1184, Université Paris-Saclay
Design and coordination of the CORIMUNO trial platform: Pr P. Ravaud, Center for Clinical Epidemiology, Hôpital Hôtel Dieu, AP-HP, CRESS, INSERM U1153, University of Paris
Statistician: Dr R. Porcher, Center for Clinical Epidemiology, Hôpital Hôtel Dieu, AP-HP, CRESS, INSERM U1153, University of Paris
Organization of the data collection: Pr M Dougados, Hôpital Cochin, AP-HP, CRESS, INSERM U1153, University of Paris
The CORIMUNO-19 clinical trials platform is promoted and funded by Assistance Publique – Hôpitaux de Paris, and supported by Inserm via its REACTing consortium (integrated into the ANRS Emerging Infectious Diseases since January 2021).
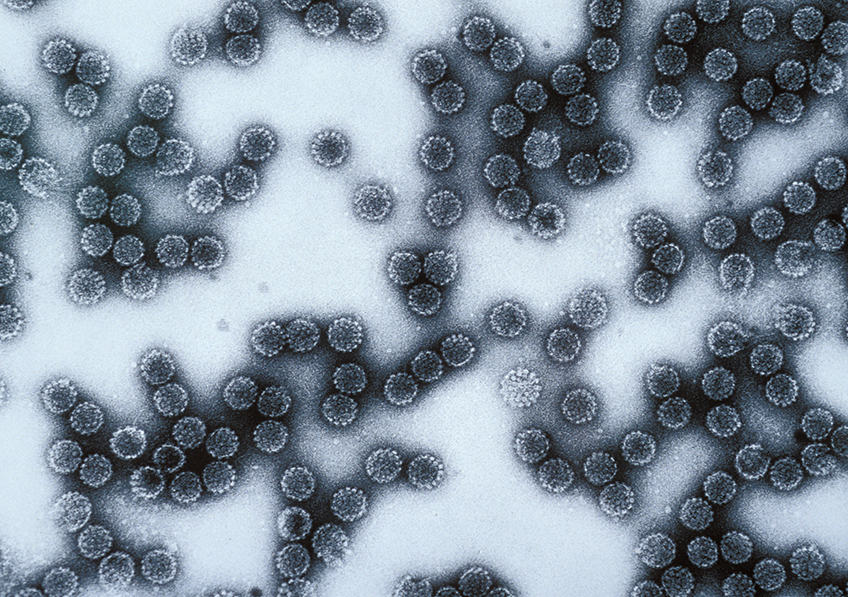
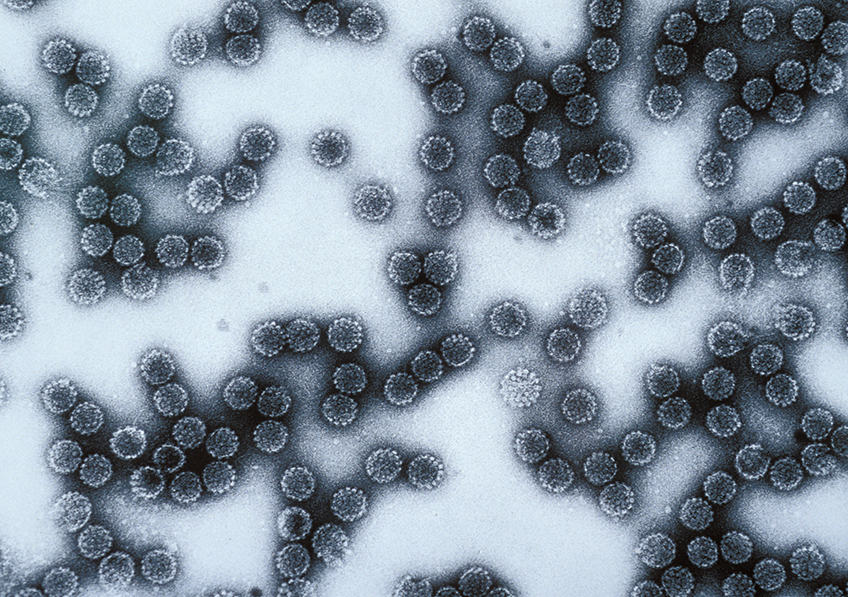
Papillomavirus. © Inserm/U190
Most of us carry human papillomaviruses (HPVs) – particularly skin papillomaviruses that generally cause warts or benign local lesions. However, on very rare occasions worldwide patients develop severe forms of these viral diseases, including “tree man” syndrome. This highly debilitating disease manifests as the uncontrolled growth of horn-like skin lesions for which surgery is ineffective. As part of an international collaboration, researchers from Inserm, teacher-researchers from Université de Paris, and doctors from AP-HP, all grouped at the Imagine Institute (Inserm/Université de Paris, Paris hospitals group AP-HP) located at Necker Hospital for Sick Children AP-HP, have been the first to reveal a genetic cause of tree man syndrome. This research was conducted by Vivien Béziat, under the supervision of Profs. Jean-Laurent Casanova and Laurent Abel, who run a laboratory with branches in Paris and New York’s Rockefeller University1. It was published on July 1, 2021, in the journal Cell.
There are over 200 human papillomaviruses (HPVs), with some causing benign skin lesions such as common or plantar warts, and others with the potential to cause cervical cancer. The Human Genetics of Infectious Diseases laboratory has focused on skin HPVs, working for several years to understand why these usually harmless infections take a severe turn in a few very rare cases.
In a publication in the journal Cell, the team of Vivien Béziat, Inserm researcher in the Human Genetics of Infectious Diseases laboratory and first author of the publication, studied the genetic characteristics of an Iranian patient with tree man syndrome, and two members of his family presenting with a severe skin HPV infection involving large numbers of warts on their hands and feet, but who had not developed the syndrome. What the three patients were found to have in common was a mutation of the CD28 gene, which usually plays a major role in activating T cells – the immune cells that destroy the cells infected by a virus.
In these patients, the CD28 gene mutation prevents the immune system from recognizing the virus and from mounting an appropriate response. The virus then proliferates in the keratinocytes, the cells that make up the skin’s epidermis, causing the uncontrolled multiplication of skin warts and/or horn-like lesions. This is the first time that a genetic cause of tree man syndrome has been identified.
However, it was when analyzing the CD28 mutation that the researchers made a different discovery. The CD28 gene, until now considered a mainstay in immune system function and T cell response, does not appear to play such a major role. The medical histories of the three patients showed exposure to several HPV types and to a very large number of other pathogens. Yet only the patient with tree man syndrome developed a severe reaction to HPV2, and only the two members of his family did so to HPV4.
“These patients only showed abnormally high susceptibility to certain papillomaviruses of the gamma-HPV and alpha-HPV genus. Based on the work done over the past 30 years, we thought that a CD28 gene dysfunction would actually make patients susceptible to many infectious agents. But even if their immune response is weakened, the patients defend themselves well against other pathogens,” explains Béziat.
“No treatment has so far been shown to be effective against tree man syndrome”. A hematopoietic stem cell transplant to replace the patient’s immune system is being considered. However, this major, costly treatment is not easily accessible to populations living in less developed countries, who will progress towards very severe forms of the disease, notably due to lack of access to care. By advancing research, the team hopes to accelerate access to treatment for these patients.
1 The Human Genetics of Infectious Diseases laboratory is directed by Jean-Laurent Casanova and Laurent Abel and is located at the Imagine Institute in Paris and Rockefeller University in New York. At both branches, Casanova heads up genetics and experimental immunology, whereas Abel heads up genetics and mathematical epidemiology.
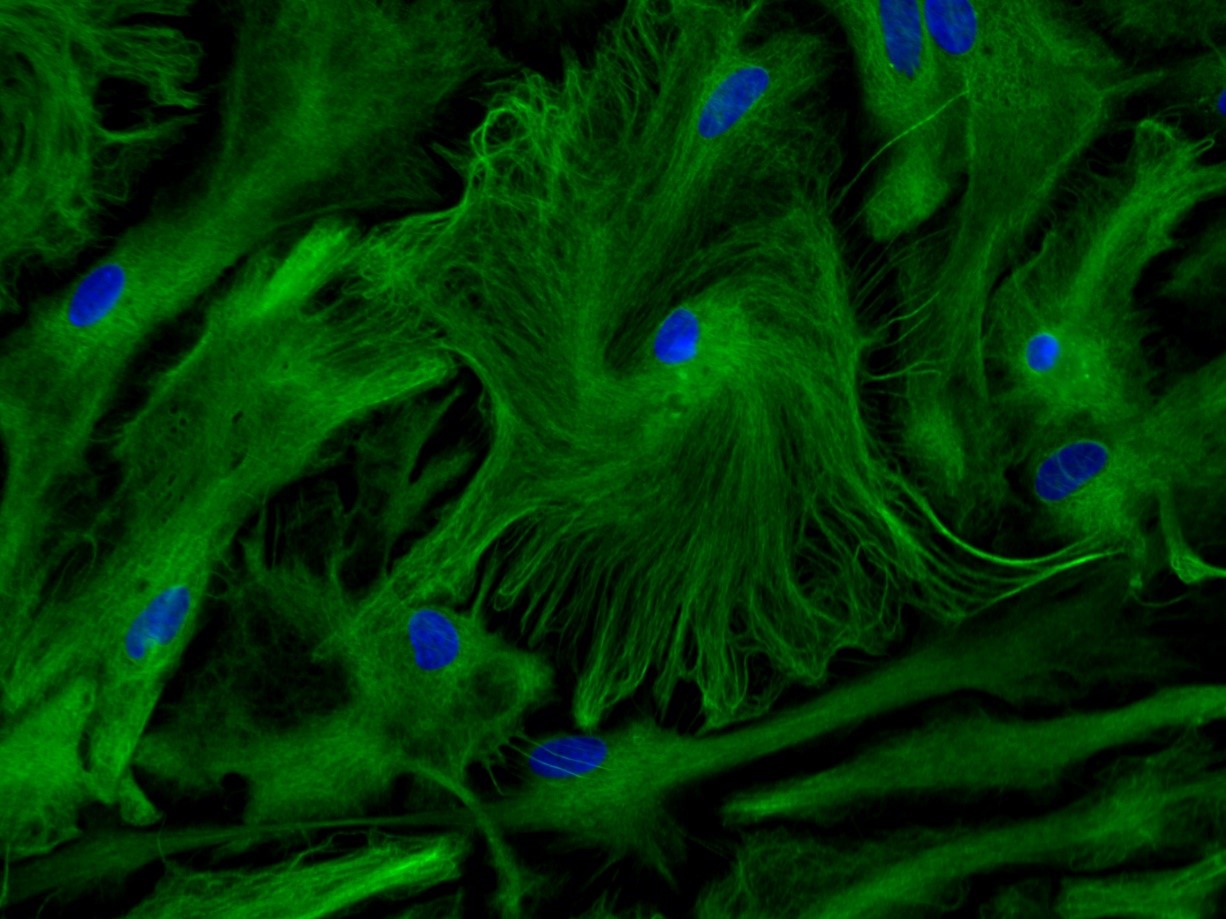
Primary culture of astrocytes © Inserm/Ruiz, Anne-Laure
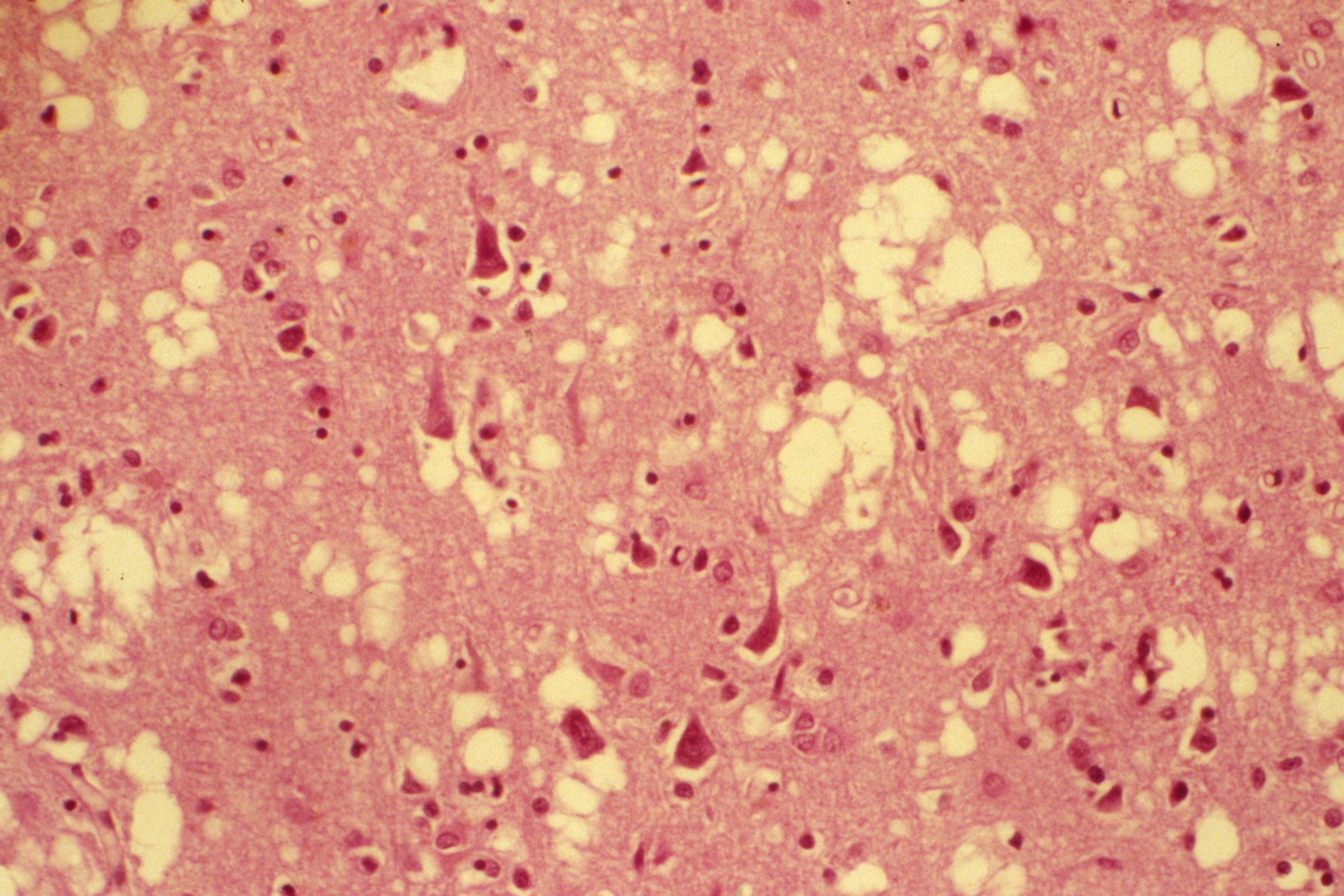
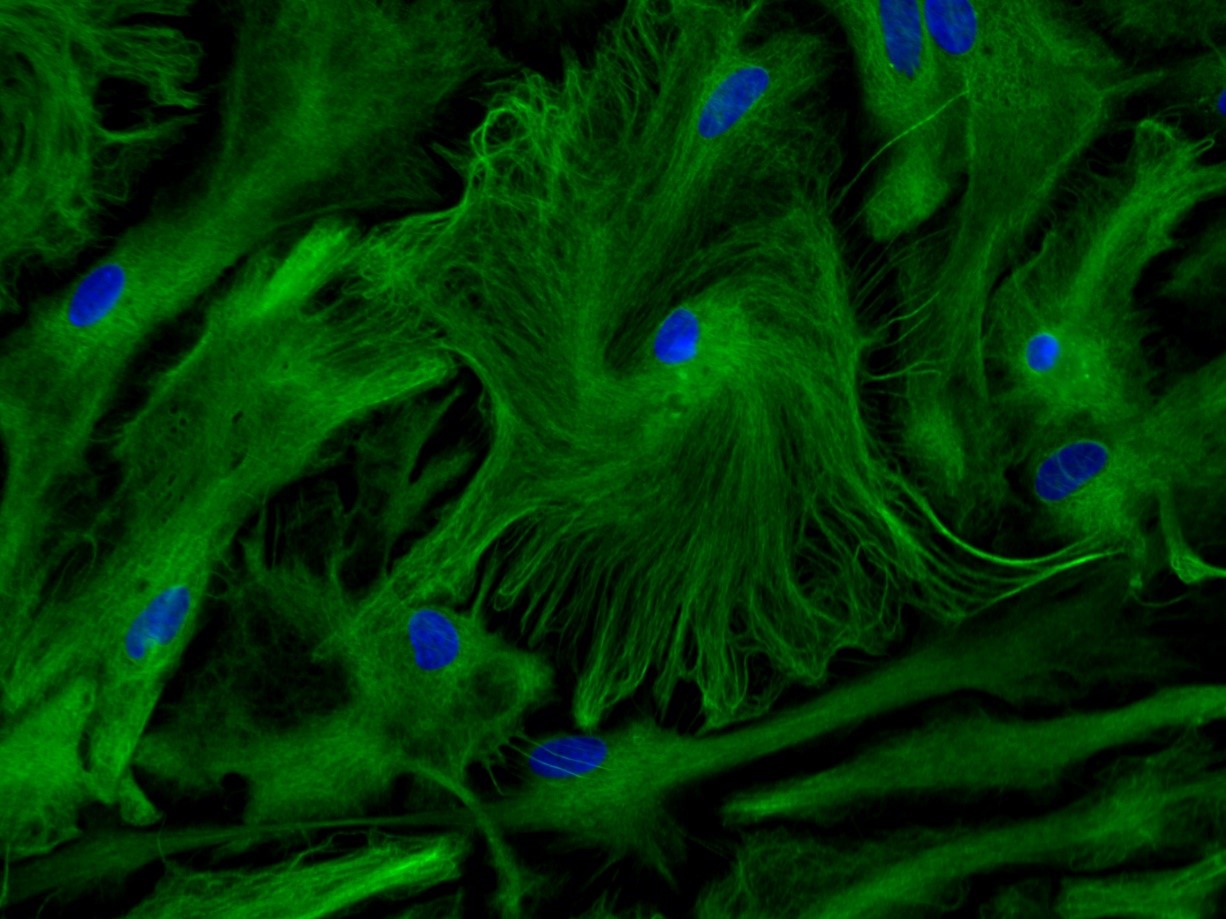
Brain plasticity is a transient key period after birth in which the brain remodels the “wiring” of the neurons according to the external stimulations it receives (environment, interactions, etc.). The end – or “closure” – of this period marks the stabilization of the neural circuits, associated with efficient information processing and normal cognitive development. Plasticity is still possible in the future, although at a much lower level than at the beginning of life.
To remedy this, the researchers aim to remodel this wiring by identifying a therapy that would reintroduce brain plasticity, even once closure has occurred. To achieve this, they also seek to better characterize the biological mechanisms that underlie this closure.
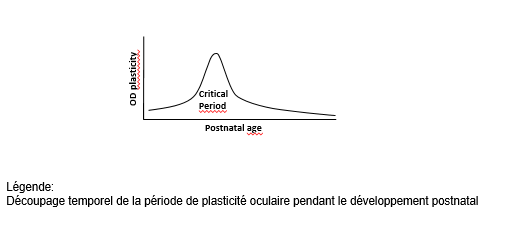
Pioneering studies from the 1980s showed that transplanting immature astrocytes into the brains of adult animals reintroduced a period of major plasticity. The team of Inserm researcher and study coordinator Nathalie Rouach at the Center for Interdisciplinary Research in Biology (Inserm/CNRS/Collège de France)[1] took inspiration from this procedure to reveal the hitherto unknown cellular process responsible for the closure of plasticity.
Through experiments on the mouse visual cortex, the researchers show that the presence of immature astrocytes is the key to brain plasticity. The astrocytes are then later involved in developing interneuron maturation[1] during the plasticity period, ultimately leading to its closure. This maturation process occurs via a novel mechanism involving the protein Connexin 30, of which the researchers found high levels in mature astrocytes during closure.
To find out, the researchers cultured immature astrocytes from the visual cortex of young mice (1 to 3 days’ old). These immature astrocytes were transplanted into the primary visual cortex of adult mice, following which the activity of the visual cortex was evaluated after four days of monocular occlusion – a standard technique used to assess brain plasticity. They found that the mice transplanted with the immature astrocytes presented a high level of plasticity, unlike the control mice which did not receive the transplant.
“This study is a reminder that in the neurosciences we must not only focus on neurons. The glial cells, of which the astrocytes are a subtype, regulate most of the brain’s functions. We realized that these cells have active roles. Glial cells are less fragile than neurons and so represent a more accessible means of acting on the brain, ” emphasizes Rouach.
[1] The interneurons establish connections between an afferent neural network (which sends information to the central nervous system) and an efferent neural network (which sends this information to the organs responding to the stimulation)


Through a critical analysis of the international scientific literature, this most recent publication takes stock of what we know about the links between exposure to pesticides and human health. © Adobe Stock
Pesticides are all products that are used to control undesirable plant species and organisms considered harmful, raising many concerns about their potential effects on human health and the environment. In 2013, at the request of the French Directorate General for Health (DGS), Inserm had published a Collective Expert Review called “Pesticides: Effects on Health”. In 2018, five ministerial directorate generals1 had tasked the Institute with updating its publication and including new topics.
The group of experts gathered by Inserm analyzed the recent scientific literature in order to examine the link between pesticides and some twenty diseases. It also analyzed the health effects of two active substances and one family of pesticides: chlordecone, glyphosate, and succinate dehydrogenase inhibitor (SDHI) fungicides.
Through a critical analysis of the international scientific literature, the 2021 Collective Expert Review takes stock of what we know about the links between exposure to pesticides and human health. It looks at neuropsychological and motor development disorders in children, cognitive disorders, anxiety and depression in adults, as well as neurodegenerative diseases and cancers in people of any age. Respiratory health, thyroid diseases, and endometriosis are also discussed. All in all, the multidisciplinary group of researchers analyzed over 5,300 documents.
For each topic, the experts studied the new epidemiological data available in order to evaluate whether there was a presumed link between the exposure of different populations to the pesticides and the onset of a disease. As in 2013, this presumed link was then graded as being strong (++), moderate (+), or weak (±). These results were then examined in relation to those of the toxicological studies, in order to evaluate the biological plausibility of the links observed.
Links established between exposure to pesticides and certain diseases
The first epidemiological studies on the subject tended to characterize exposure to pesticides without precisely distinguishing the family of pesticides or the active substance. They often concerned people who in principle were most exposed due to having regularly handled such products as part of their work. More recent studies have sought to specify the disease subtypes (for example, the different types of leukemia), identify the active substances involved or investigate the link with populations supposedly less exposed than those who work with pesticides, such as those living near agricultural areas, the general population, or more sensitive populations such as children.
The expert review confirms a strong presumed link between occupational exposure to pesticides and four diseases: non-Hodgkin lymphomas (NHLs), multiple myeloma, prostate cancer, and Parkinson’s disease. It also highlights the strong presumed link between occupational exposure to pesticides and two other diseases: cognitive disorders and chronic obstructive pulmonary disease (COPD)/chronic bronchitis (see boxed text).
A moderate presumed link has also been revealed between exposure to pesticides, mainly in an occupational context, and Alzheimer’s disease, anxiety, depression, certain cancers (central nervous system, bladder, kidney, leukemia, soft tissue sarcomas), asthma and thyroid diseases.
A closer look at the six adult diseases for which a strong presumed link has been established with occupational exposure to pesticides
Non-Hodgkin lymphoma (NHL): links between exposure to malathion, lindane, DDT, and organophosphates (++) had been identified in 2013. Recent data support a stronger presumed link in 2021 for diazinon (++) and chlordane (+). For glyphosate, the presumed link is reinforced for occupational exposure (+). A weak presumed link has been reported for the first time with dicamba (±). The data also suggest links between NHL subtypes and certain pesticides.
Multiple myeloma: for the first time, links with active substances have been revealed for permethrin (+) and for carbaryl, captan, DDT, and glyphosate (±).
Prostate cancer: this analysis reinforces the role mentioned in 2013 of occupational exposure to certain organophosphate insecticides, such as fonofos (+) and highlights that of terbufos (+) and malathion (+) as well as an organochlorine insecticide (aldrin, +). It emphasizes a higher risk of developing an aggressive form of the disease, suggesting a possible role in the progression of the disease and not only in its onset. For chlordecone, the expert review considers there to be a strong presumed link (++) and that a causal relationship is likely.
Parkinson’s disease: the data confirm the link with paraquat (+) and new studies suggest weak presumed links (±) with active ingredients of the dithiocarbamate fungicide family (zineb, ziram and mancopper). The new studies on the exposure of people living near agricultural areas suggest a weak presumed link with pesticides in general.
Cognitive impairment: the presumed link increased from moderate to strong (++) with exposure to pesticides, mainly organophosphates, in farmers. The most recent studies have been extended to include people living near agricultural areas or the general population and consider the presumed link to be moderate (+).
Respiratory health (not covered in 2013): a strong presumed link between occupational exposure to pesticides and the onset of COPD and chronic bronchitis has been established. Seventeen active substances were found to be associated with a disease or the impairment of a respiratory function parameter, with the majority having a weak presumed link (±). To evaluate the biological plausibility of this link, three effects were studied in a toxicology setting (oxidative stress, mitotoxicity, and immunomodulation) and among these 17 pesticides, 11 are associated with at least two toxicological effects and two, permethrin and chlorpyrifos, with all three effects.
Certain periods of life such as pregnancy and early childhood are more vulnerable in the face of a toxic event or agent.
The recent results have made it possible to specify the type of pediatric leukemia concerned during exposure of the mother during pregnancy: acute leukemia and domestic uses (strong presumed link) and acute myeloid leukemia and occupational exposure. A new link has been found between the risk of acute lymphoblastic leukemia in case of paternal occupational exposure in the preconception period (moderate presumption).
Concerning central nervous system tumors, the expert review confirms the strong presumed link between the occupational exposure of the parents to pesticides (without distinction) during the prenatal period. In addition, the recent results lead to a strong presumed link between central nervous system tumors and domestic exposure to pesticides (without distinction) during pregnancy or childhood.
Other research focuses on the links between occupational or environmental exposure of mothers during pregnancy and neuropsychological and motor developmental disorders in children. They confirm the existence of a strong presumed link, especially for certain families of pesticides, such as the organophosphates. Regarding the pyrethroids, whose use has increased as a replacement for organophosphate insecticides, the results of new studies are consistent and show a link between pyrethroid exposure during pregnancy and an increase in internalized behavioral problems such as anxiety (strong presumed link). Toxicological data support the biological plausibility of an effect based on the modes of action of these pesticides.
Consider the most recent scientific data to better protect populations
The confirmation and highlighting of strong presumed links between certain diseases and exposure to pesticides should encourage the authorities to take better account of these issues. In addition, the scientific literature on the subject is raising new concerns, particularly regarding the indirect effects of certain pesticides on human health through their effects on ecosystems, which should be taken into account more by researchers and decision-makers.
What can be said about chlordecone, glyphosate and SDHIs?
1 The Directorates General for Risk Prevention, Health, Labor, Research and Innovation, and the Secretary General of the Ministry of Agriculture and Food


BioCluster©ParisSaclay
Sanofi, Gustave Roussy, Inserm, Institut Polytechnique de Paris and the University of Paris-Saclay are committed to developing personalized medicine in France through a patient-centered oncology cluster – the Paris Saclay Cancer Cluster.
Following the announcements made by French President Emmanuel Macron at the Strategic Council for Health Industries, Sanofi, Gustave Roussy, Inserm, Institut Polytechnique de Paris and the University of Paris-Saclay have announced plans to create the Paris Saclay Cancer Cluster, a center bringing together key players in oncology innovation. This project, which is unique in Europe, will bring together the best scientific, human and technological expertise to shape the future of personalized medicine and accelerate the discovery of new customized cancer treatments. Within ten years, the objective is to be able to offer rapid diagnosis at the patient’s bedside, including disease modeling and the construction of an individualized and personalized therapy.
Oncology is a field where the medical needs of patients remain largely unmet and where innovations must lead to improved diagnosis, treatment and survival. Ensuring that France and Europe are leaders in oncology innovation in 2030 is a key challenge. France has world-renowned strengths in oncology (quality of academic research with a number of publications that ranks France 2nd in the world, hospitals, industrial companies, venture capital funds, incubators); these assets must lead to the emergence of therapeutic and diagnostic solutions that will transform the lives of patients and enable the emergence of a truly global innovation ecosystem.
The Paris Saclay Cancer Cluster project aims to build on this high-potential ecosystem by bringing together the key players in oncology innovation (patients, hospitals, universities, pharma companies, investors, national research organizations, patient associations and public authorities) to develop the most effective synergies. With strong political support, the project will lead to the creation of a Prospective Oncology Center in the Paris region.
The Paris Saclay Cancer Cluster would stand out with:
“The Paris Saclay Cancer Cluster intends to be both unique and complementary to existing facilities through its research strategy, which integrates all dimensions – clinical, fundamental, academic, industrial, transdisciplinary, etc. – on a single theme, located in a single location, as close as possible to patients. The ambition of this major project is to enable France and Europe to become world leaders in cancer research,” said Professor Jean-Charles Soria, CEO of Gustave Roussy.
“Improving the care of cancer patients is fundamental for Sanofi. Facing an opponent as challenging as cancer, I am delighted that public and private players bringing together the best medical, academic, and scientific expertise, join forces to advance research and create a European dynamic. The convergence of biology and medicine with data science and artificial intelligence offer major opportunities to accelerate therapeutic innovation and create future leading companies in oncology, positioning France at the forefront of innovation in Europe and the world,” said Paul Hudson, Chief Executive Officer of Sanofi.
“I am delighted with this strong impetus that will combine the best of academic research with ambitious industrial development and will fully contribute to scientific advances in the fight against cancer,” said Dr. Gilles Bloch, President and CEO of Inserm.
” The University of Paris-Saclay is very pleased to be a founding member of the Paris Saclay Cancer Cluster, which is part of a will to respond with our industrial partners to one of the major challenges of our time. This common trajectory with our faculties of medicine and pharmacy irrigates training, research and innovation in cancerology. The University’s high disciplinary level in this field is enriched by interfaces in AI, data sciences, applied mathematics and engineering, also at the highest world level,” said Sylvie Retailleau, President of Université Paris-Saclay.
“By participating in the creation of the Paris Saclay Cancer Cluster, Institut Polytechnique de Paris affirms its strong commitment to a major challenge facing our society, cancer research, by contributing its skills in AI, data science and engineering. This union of all the public and private players around a great ambition, allowing us to bring innovations in this field to scale, will help our country achieve its therapeutic sovereignty,” said Eric Labaye, President of Institut Polytechnique de Paris.
Next steps
After a preparation and scoping phase, the first projects of the cluster should start by the end of 2021. They will focus on identifying new therapeutic targets based on a large collection of patient samples. Beforehand, a legal structure that will host the Paris Saclay Cancer Cluster will be created and its first employees, including its Managing Director, will be recruited, while the technological platforms, data and first training courses will be accessible (via the Cluster) from 2021/2022. The founders are already meeting with various players in the fields of oncology, data and AI, who could join the cluster in the near future.
From 2023/2024, the opening of the Prospective Oncology Center on a site close to Gustave Roussy will mark a real acceleration for the cluster: the objective will be to select at least ten new projects per year.
After 2025, the cluster will enter a phase of sustainability and expansion, notably through the emergence of projects focused on the creation and optimization of new treatments and drugs and their development (accelerated and facilitated by artificial intelligence), on the invention of new administration systems to provide patients with personalized treatment, and on the deployment of innovative treatment methods directly at their bedside, while disseminating these models so that they benefit all patients regardless of where they are treated in the territories.
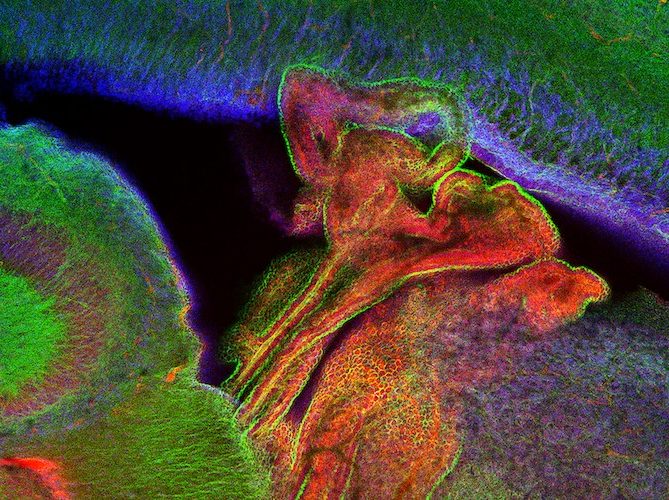
© Choroid plexus of mouse neonates. Blue: cell nuclei, green: phalloidin-actin, red: fluorochrome. Credits: Biology of Infection Unit, Institut Pasteur
Meningitis is associated with high mortality and frequently causes severe sequelae. Newborn infants are particularly susceptible to this type of infection; they develop meningitis 30 times more often than the general population. Group B streptococcus (GBS) bacteria are the most common cause of neonatal meningitis, but they are rarely responsible for disease in adults. Scientists from the Institut Pasteur, in collaboration with Inserm, Université de Paris and Necker-Enfants Malades Hospital (AP-HP), set out to explain neonatal susceptibility to GBS meningitis. In a mouse model, they demonstrated that the immaturity of both the gut microbiota and epithelial barriers such as the gut and choroid plexus play a role in the susceptibility of newborn infants to bacterial meningitis caused by GBS. The findings were published in the journal Cell Reports on June 29, 2021.
Newborn infants are more likely to develop bacterial meningitis than children and adults. Group B streptococcus (GBS) is the pathogen responsible for a significant proportion of cases of neonatal meningitis. In most instances, infection is preceded by bacterial colonization of the gut. The commensal bacterial gut flora (known as the microbiota) plays a key physiological role, as it is involved in digestion, offers protection from gut pathogens and contributes to tissue differentiation and immune development. Newborns have no gut microbiota; it gradually develops in the first few weeks after birth.
In a new study, scientists from the Institut Pasteur, in collaboration with Inserm, Université de Paris and Necker-Enfants malades Hospital (AP-HP), demonstrated in a mouse model that the immaturity of the gut microbiota in neonates is involved in neonatal susceptibility to meningitis caused by GBS. In the absence of a mature microbiota, the bacteria can extensively colonize the gut. In the absence of a mature microbiota, the barrier function of blood vessels in the gut that the bacteria must cross to reach the brain through the bloodstream is also less effective, and the immune system is unable to control infection.
“In this study, we show how two factors associated with infancy – the immaturity of the gut microbiota and the growth of gut and choroidal epithelial tissues – play a role in the susceptibility of newborn infants to meningitis caused by GBS, at all stages of infection from gut colonization to dissemination in the brain,” explains Marc Lecuit (university professor/hospital practitioner, Université de Paris and Necker-Enfants Malades Hospital), head of the Biology of Infection Unit at the Institut Pasteur and Inserm and last author of the study.
The results of this research illustrate the importance of the microbiota and its critical role in protecting against infection.